The purpose of disability slips is to advise the employer when the medical provider does not believe the injured employee can do any work in their current medical status or is able to work only in a restricted capacity. Running an effective workers’ compensation program requires employers and other interested stakeholders have clarity, conform to the law, and help get that employee back to work promptly.
Demanding the Basics for Injured Employee Disability
The quality of the disability slips covers the spectrum from telling the employer everything about the injured employee’s injury and disability, to telling them nothing at all. The lack of uniformity can create issues for the employer in tracking the status of the injured employees.
Click Link to Access Free PDF Download
Some jurisdictions have minimum requirements when it comes to disability slips following a work injury. Florida’s Division of Workers Compensation mandates every medical provider use the same Medical Treatment Status Reporting Form, DWC-25. This form serves two purposes. It requires the health care provider to outline the functional status of an injured employee, and report their treatment plan. Even if a jurisdiction does not require a form to be completed, the interested stakeholder can take proactive action to demand it.
Avoid Employee-Determined “Off-Work” Status
When the medical provider does not provide the “off-work” slip, and the employer does not ask, the employee becomes the person determining when the employee will return to work. This is not a good situation for all interested stakeholders and turns workers’ compensation into an entitlement program. Proactive employers should require a disability slip be turned in by the employee after every medical appointment. This information encourages timely return-to-work and holds everyone accountable.
In some jurisdictions, the state department overseeing the workers’ compensation program can help employers obtain this information. In Minnesota, a Health Care Provider Report is required to be completed and returned within 10 days of receipt by a medical provider. The Department of Labor and Industry will follow-up with medical providers when such form is submitted. Failure to respond can result in a penalty being assessed against the medical provider.
Take Charge with the Medical Provider
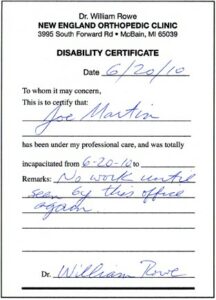
If the medical provider treating the employee is sending an off-work slip that states “no work until seen by this office again,” with no further information, the employer needs to take charge and advise the medical provider’s office more information needs to be provided. At a minimum, the off-work slip should provide the date of the next office visit and the employee’s current physical limitations. Basic information that should always be included should have the following:
- The employee’s name
- The date of the office visit
- Whether the office visit was work-related
- Objective findings
- Diagnosis and prognosis
- The existence of a pre-existing condition
- The specific nature of any functional limitations, for example:
- No bending
- No carrying over ____ pounds
- No climbing
- No kneeling
- No lifting over _____ pounds
- Standing limitation ________
- Sitting limitation _________
- Walking limitation _________
- Other relevant limitations
- Date of next office visit
- Anticipated full duty date
- Anticipated date of Maximum Medical Improvement (MMI)
- Date of next appointment
- Anticipated treatment plan
- Doctor or health care providers signature
FREE DOWNLOAD: “5 Critical Metrics To Measure Workers’ Comp Success”
Help Me, Help You!
Medical providers are in the business of providing medical care, and often have no knowledge about the employer’s business. It is important for employers to let medical providers know about their business and the employee’s pre-injury position. Relevant information to send can include a job description or video of the work the employee will be expected to perform. This will allow the doctor or health care provider to better understand the employee’s job and its physical requirements.
Conclusions
Employers need to take the lead when it comes to returning employees to work following a work injury. One important step in this process is making sure health care providers are properly completing disability slips with specifies about the employee’s restrictions and/or limitations. By demanding this information, employers can receive a more honest assessment of the employee’s ability to work rather than letting the employee drive their time off work. It will also reduce workers’ compensation program costs in the long run.

Contact: mstack@reduceyourworkerscomp.com.
Workers’ Comp Roundup Blog: https://blog.reduceyourworkerscomp.com/
©2019 Amaxx LLC. All rights reserved under International Copyright Law.
Do not use this information without independent verification. All state laws vary. You should consult with your insurance broker, attorney, or qualified professional.
FREE DOWNLOAD: “5 Critical Metrics To Measure Workers’ Comp Success”