As of July 2022, the United States has nearly 50 million confirmed cases of COVID-19 infections, with more than 1 million deaths. There are several published studies that have reported varying percentages of COVID-19 infected individuals who subsequently endured persistent, debilitating symptoms for weeks and months after initial infection. This is regardless of the severity of illness originally experienced, whether mild or severe. Many have referred to this medical condition with prolonged symptoms as “long COVID,” “long-haul COVID,” “chronic COVID,” and “post-acute sequelae of SARS CoV-2 infection (PASC).” This study takes a first look at long COVID (i.e., PASC) experience in workers compensation (WC).
KEY FINDINGS
- The percentage of COVID claims with long COVID in WC was 24%
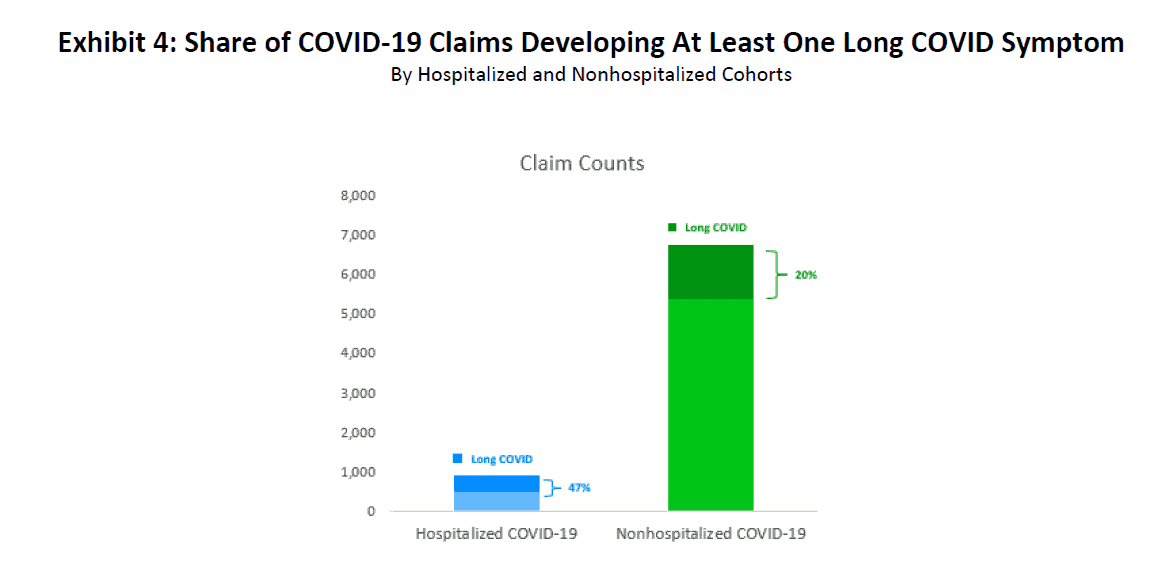
- Twenty percent (20%) of nonhospitalized and 47% of hospitalized COVID-19 WC patients developed long COVID
- Hospitalized patients who developed long COVID took longer for such symptoms to resolve compared to patients who were not admitted to the hospital
- The most common symptoms seen in long COVID patients were of a pulmonary or cardiovascular nature
- Hospitalized patients sought more physical medical services in the 30- to 270-day PASC window than nonhospitalized patients
- Home health care services performed in the 30- to 270-day PASC window were among the top three medical services provided for patients who had been hospitalized
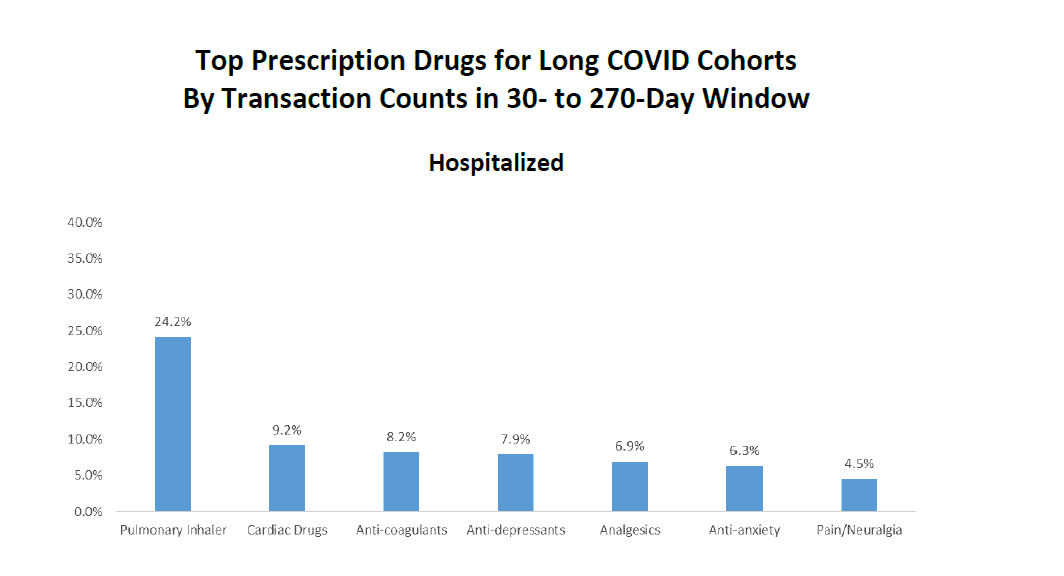
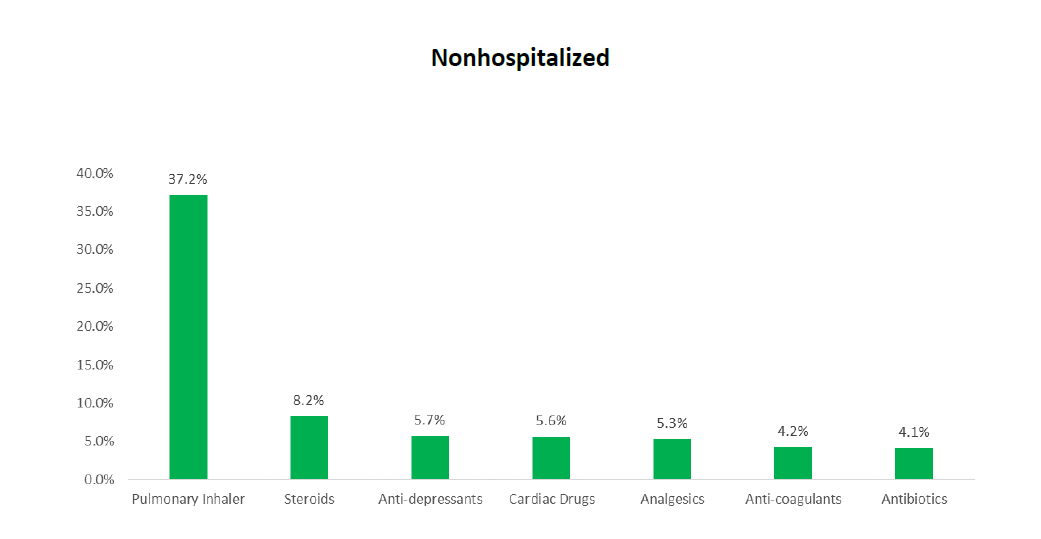
- Prescriptions for pulmonary inhalers dominated both the hospitalized and nonhospitalized cohorts
- The average temporary disability indemnity benefit duration for long COVID patients was about 160 days for hospitalized patients and 95 days for nonhospitalized patients
BACKGROUND
The National Institutes of Health (NIH) assigned the term “post-acute sequelae1 of SARS-CoV-2 infection (PASC)” to enable research initiatives to better understand etiology and optimal treatment approaches for the prolonged constellation of symptoms beyond the acute COVID-19 infection period. While there is no standardized or universal definition of long COVID or PASC, the Centers for Disease Control and Prevention (CDC) characterizes it as “an umbrella term for the wide range of health consequences that are present four or more weeks after infection with SARS-CoV-2.” In October 2021, Dr. Michael Choo of Paradigm, in conjunction with NCCI, published the first of this two-part research regarding long COVID titled “COVID-19 and The New Reality – Prolonged COVID,” which outlined the potential disability implications of long COVID on the WC industry.
A systematic review of medical studies on the long COVID burden among COVID-19 survivors published in the Journal of the American Medical Association (JAMA) indicated that the median frequency of long COVID was 54%, 55%, and 54% at 1 month, 2–5 months, and 6+ months post-COVID-19 infection, respectively [1]. The CDC reports that one in five COVID-19 survivors aged 18–64, and one in four survivors at least 65 years of age, experienced an incident condition that might be attributable to a previous COVID-19 illness [2].
This report follows up on “COVID-19 and The New Reality – Prolonged COVID” and reports on preliminary trends and potential impacts of long COVID in WC from the perspective of both medical and indemnity costs. There are two considerations regarding the results contained in this analysis:
- Data used for this report extends through the first quarter of 2022 (for claims with accident dates between March 2020 and June 2021). Thus, data does not fully reflect the potentially longer-term impacts of long COVID.
- The findings in this report are largely observational, rather than inferential. Furthermore, there are several confounding factors that could not be controlled for, preventing statistically rigorous Such factors include:
- Impact of COVID-19 presumptions or other legislative changes affecting the compensability of COVID-19 claims in the WC system
- The degree to which settlement of future medical benefits2 occurs in each state
- The presence and effectiveness of mask mandates, social distancing, business shutdowns, and vaccination rates across states
- The evolution of treatment protocols
1 “Post-acute sequelae” refers to a condition that is the consequence of a previous disease or injury.
2 Lump-sum payments are not reported in NCCI’s Medical Data Call. In states where a significant portion of medical benefits are paid as lump-sum settlements, the data available for this report is censored.
DATA
The data sources used in this report are NCCI’s Indemnity Data Call (IDC) and Medical Data Call (MDC), which include WC experience for covered employers other than self-insured entities. Both include data reported by all WC carriers that write at least 1% of the market share in any one state for which NCCI collects indemnity and medical data.3
- The IDC is a collection of transaction-level detail for indemnity benefit payments, as well as summarized paid and incurred-to-date information evaluated on a quarterly basis. Subject to the above conditions, the IDC consists of claims for which an indemnity payment has been made or an indemnity reserve established.
- The MDC is a collection of paid transactions to medical providers for services provided. Medical transactions are reported for each WC claim until the claim is closed or until 30 years from the accident However, lump-sum payments or payments in bulk are not systematically reported.
IDC data used in this report consists of:
- Data reported for claims with accident dates from March 1, 2020, through June 30, 2021
- COVID-19 claims identified based on reporting of Cause of Injury Code 83 (Pandemic)
MDC data used in this report consists of:
- Data reported for medical services provided from March 1, 2020, through March 30, 2022, for claims with accident dates between March 1, 2020, and June 30, 2021
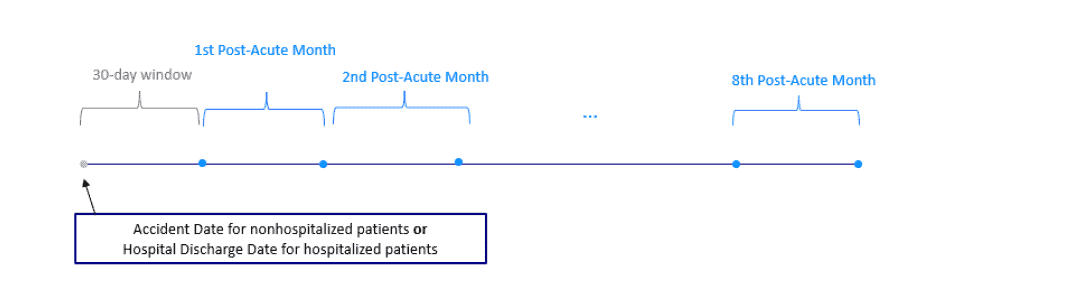
To observe consistent time frames for all claims, we are interested in examining medical transactions for the nine months following the accident date (for those affected workers not hospitalized) or nine months following the initial discharge date (for those hospitalized). Therefore, the latest accident date that can be included is June 30, 2021.
Claims identified as COVID-19 in the IDC are linked to the corresponding claims in the MDC to extract the Medical data transactions for reported COVID-19 claims. The resulting data does not include:
- medical-only claims
- indemnity-only claims (i.e., “quarantine claims”)
The total number of COVID-19 claims underlying this analysis is 7,651, and the associated payments are $40.9M in indemnity and $79.6M in medical.
For hospitalized patients, this study defines a long COVID claim as one that has at least one occurrence of one of the ICD- 104 codes listed in Appendix A beyond 30 days but less than or equal to 270 days from the initial hospital discharge date.
Similarly, for nonhospitalized patients, a claim is defined as a long COVID claim if there is at least one of the aforementioned ICD-10 transactions beyond 30 days but less than or equal to 270 days from the accident date. The 30-day window immediately following the hospital discharge or accident date is not considered in defining a long COVID claim. This effectively gives each COVID-19 claim an eight-month observation period to be evaluated for symptoms associated with long COVID.
More than 150 ICD-10 codes associated with long COVID are grouped into the following eight symptom groups:
- Pulmonary
- Cardiovascular
- Neurological
- Systemic
- Endocrine
- Autoimmune
- Mood
- Sleep Disorders
The MDC has primary and secondary ICD-10 fields. If a long COVID symptom group associated with the primary ICD-10 differs from the symptom group of the secondary ICD-10, the primary ICD-10 is chosen. If the primary ICD-10 is not associated with any of the long COVID symptom groups, but the secondary ICD-10 is, then the secondary ICD-10 code and its grouping are chosen.
Following are some of the terms and metrics used in this paper:
- Hospitalized—COVID-19 claims with at least one inpatient hospital admission, with each hospitalization lasting at least 48 hours. The post-acute sequelae period is defined as > 30 days and < 270 days from the discharge date of the initial hospital admission.
- Nonhospitalized—COVID-19 claims without any hospital Post-acute sequelae period is defined as > 30 days and < 270 days from the accident date.
- 30- to 270-day window—A time period starting 30 days and ending 270 days from the initial discharge date/accident date for hospitalized/nonhospitalized patients. The length of this window is eight months.
- Long COVID claim—A COVID-19 claim that had at least one occurrence of ICD-10 codes defined in Appendix A in the 30- to 270-day window.
- No long COVID claim—A COVID-19 claim that does not have any symptoms that are associated with long COVID in the 30- to 270-day window. While such claims may include less severe cases of COVID-19, they may also include severe claims that do not include symptoms associated with long COVID in the 30- to 270-day window (e.g., organ failure, stroke, and heart attack).
3 States used in this study are AK, AL, AR, AZ, CO, CT, DC, FL, GA, HI, IA, ID, IL, IN, KS, KY, LA, MD, ME, MN, MO, MS, MT, NC, NE, NH, NM, NV, OK, OR, RI, SC, SD, TN, TX, UT, VA, VT, WI, and WV.
4 International Classification of Diseases (ICD) is a globally used diagnostic tool for epidemiology, health management, and clinical purposes.
EXHIBITS
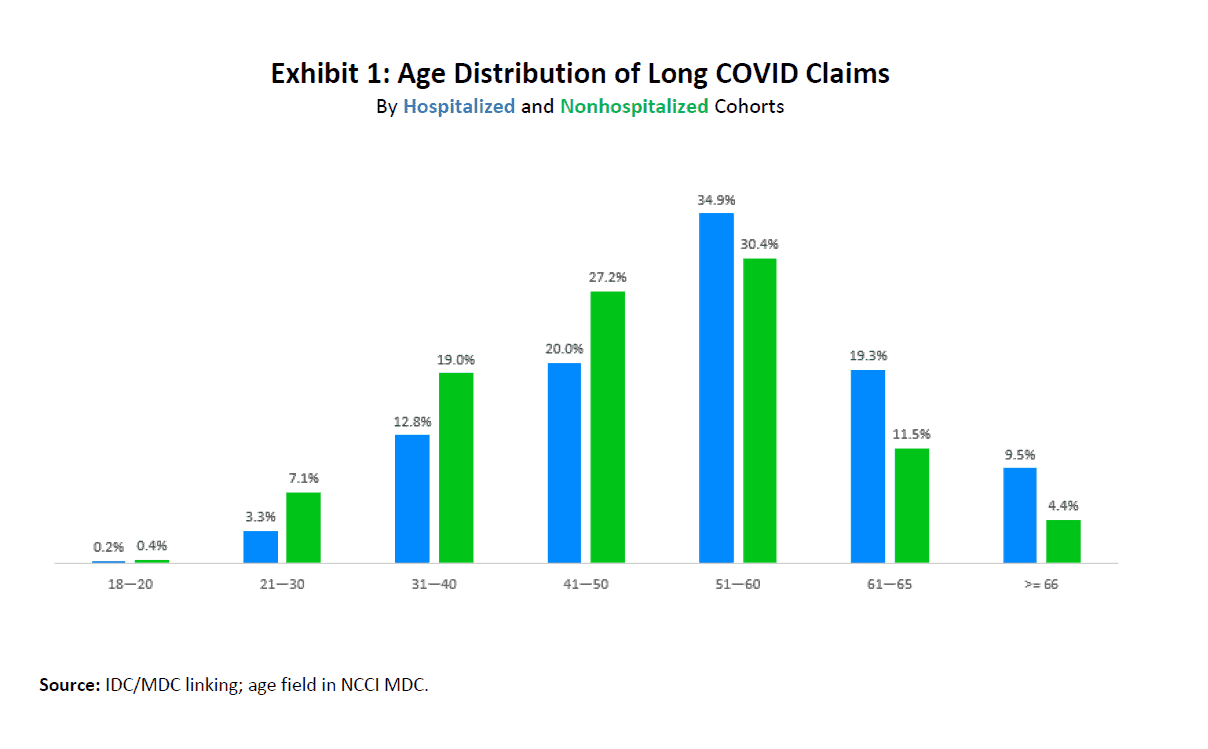
Exhibit 1 shows the age distribution of long COVID claims, broken down into hospitalized and nonhospitalized cohorts.
Fewer than half of the nonhospitalized long COVID patients were older than 50. Nearly 64% of hospitalized patients were older than 50, and just under 10% were 66 years old and older.
Because we now know that the risk of severe illness from COVID-19 increases with age, it is not surprising that the older age groups represented a greater share of the hospitalized long COVID claims.
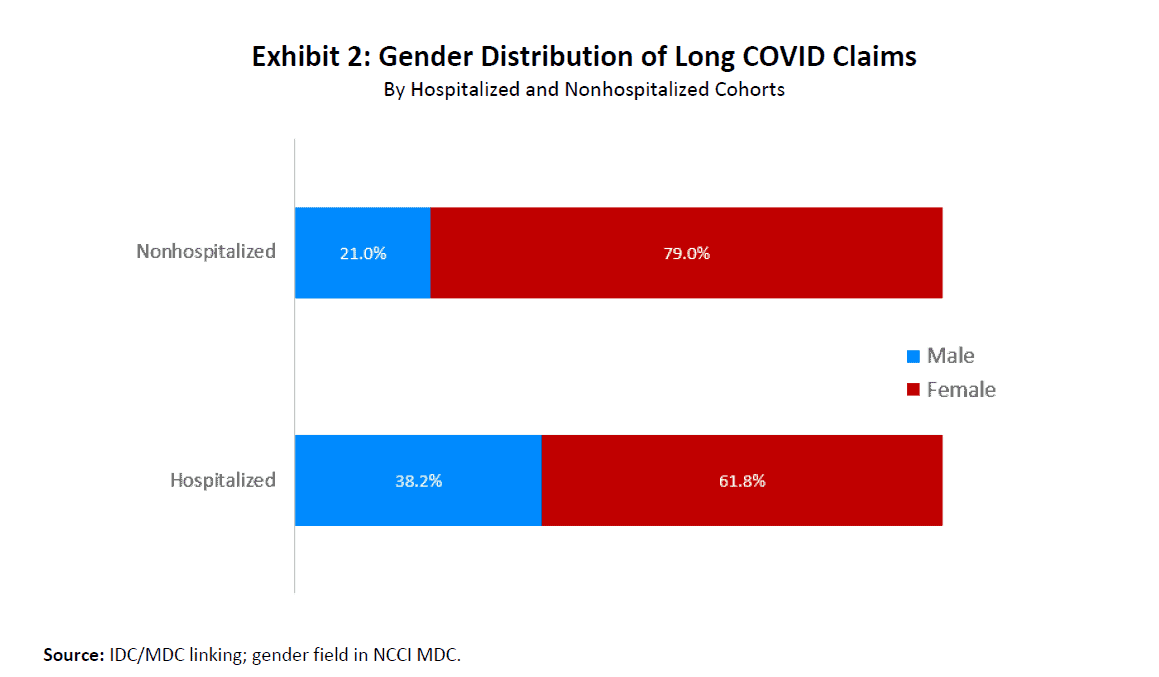
Exhibit 2 shows that for the nonhospitalized long COVID cohort, females outnumbered males by almost 4 to 1. Females were also over-represented in the hospitalized cohort, although to a lesser extent.
One possible explanation for the higher share of males hospitalized when compared to those who are not hospitalized is that men tend to have more cardiovascular diseases [3], which may lead to more severe illness and hospitalizations.
Additionally, a larger share of adult males are smokers [4].
But how does one explain the higher representation of females in both cohorts? To answer that question, we need to look at the occupations that COVID-19 most impacted in WC.
While the pandemic has impacted a wide cross-section of people across the country, frontline workers experienced the brunt of work-related COVID-19 [5]. This also holds true for long COVID claims because healthcare workers and first responders dominate the top 10 long COVID class codes in WC.
As seen in Exhibit 3, Code 8833—Hospital—Professional Employees was the NCCI classification code with the largest percentage of long COVID claims, at almost 30%. Code 8824—Retirement Living Centers—Health Care Employees follows at nearly 12%. These occupational groups employ a relatively high percentage of women and combined to account for nearly 42% of long COVID claims in the data analyzed.
After subtracting the 5.9% share for Class Code 8810, which is the only code among the top 10 that is neither related to a healthcare nor a first responder code, the remaining 9 class codes comprised just over 80% of long COVID claims.
Exhibit 3: Top 10 Long COVID Class Codes
By Share of Long COVID Claims
| Class Code* | Description | Share of Long COVID Claims |
| 8833 | Hospital—Professional Employees | 29.7% |
| 8824 | Retirement Living Centers—Health Care Employees | 11.9% |
| 8832 | Physician and Clerical | 9.7% |
| 8829 | Convalescent or Nursing Home—All Employees | 8.0% |
| 8835 | Home, Public, and Traveling Healthcare—All Employees | 6.2% |
| 8810 | Clerical Office Employees | 5.9% |
| 9040 | Hospital—All Other Employees | 5.3% |
| 8826 | Retirement Living Centers—All Other Employees, Salespersons and Drivers | 4.2% |
| 7705 | Ambulance Service Companies and EMS—Providers and Drivers | 3.2% |
| 7720 | Police Officers and Drivers | 2.0% |
* Item B-1436 may impact data reported in Codes 8824 and 8829. Reporting in these codes will vary across states based on
(1) applicability of Item B-1436 in each state and (2) experience filing effective dates by state.
Source: IDC/MDC linking; NCCI’s Statistical Plan at first report.
Measuring the long COVID prevalence rate is an important task for the WC industry. Exhibit 4 shows that almost half of hospitalized COVID-19 patients had at least one symptom 30 days after the initial discharge. For the nonhospitalized cohort, one out of five patients received treatment for long COVID symptoms. These numbers are consistent with the published research available with long COVID prevalence ranging from 20%–55% [1], [2], [6].
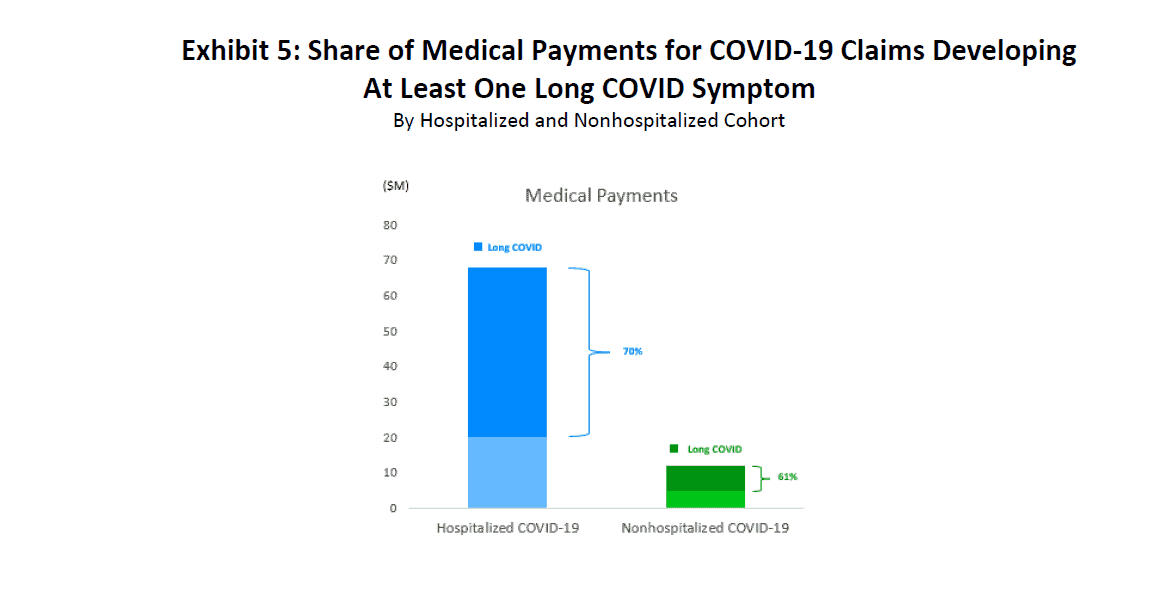
In Exhibit 5, we observe that medical payments5 associated with claims that developed long COVID symptoms made up anywhere from 60% to 70% of total medical payments for COVID-19 claims, depending on hospitalization status.
5 Medical payments include payments made during the acute phase as well as during the 30- to 270-day window.
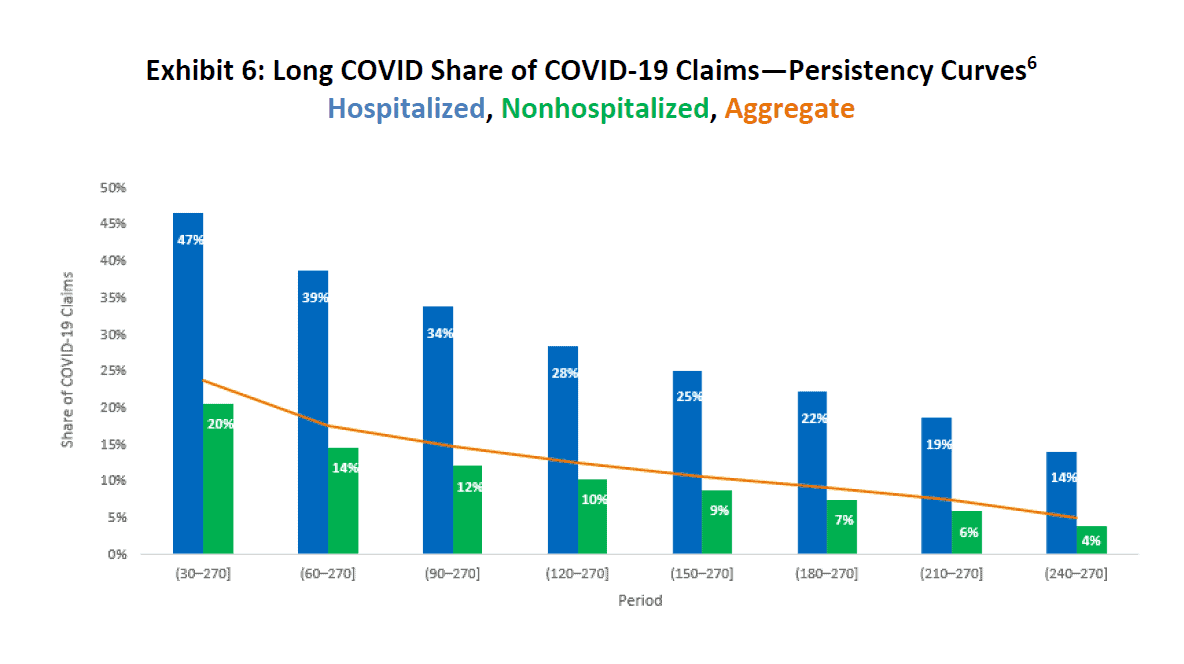
While Exhibit 4 shows the overall share of COVID-19 claims exhibiting long COVID symptoms beyond 30 days of hospital discharge or accident date, Exhibit 6 calculates the same metric but uses threshold points in increments of 30 days. For example, as of 30 days, 47% of hospitalized COVID-19 patients and 20% of nonhospitalized patients had persisting long COVID symptoms, resulting in an average of 24% altogether. By 270 days, only 14% of hospitalized COVID-19 patients and 4% of nonhospitalized patients continued to have symptoms.
Exhibit 6 also shows that, at any point in our study, a hospitalized patient was more likely to exhibit symptoms associated with COVID-19 than a patient in the nonhospitalized cohort.
Source: IDC/MDC linking. The bar values indicate the percentage of COVID-19 claims having at least one transaction from eight symptom groups in the appropriate period. Share of long COVID claim counts for the 30–270 period (47% for hospitalized and 20% for nonhospitalized) balances to values in Exhibit 4.
6 A conditional persistency curve is included in Appendix B, which shows the likelihood that long COVID patients at certain thresholds will continue to have long COVID symptoms in future time periods.
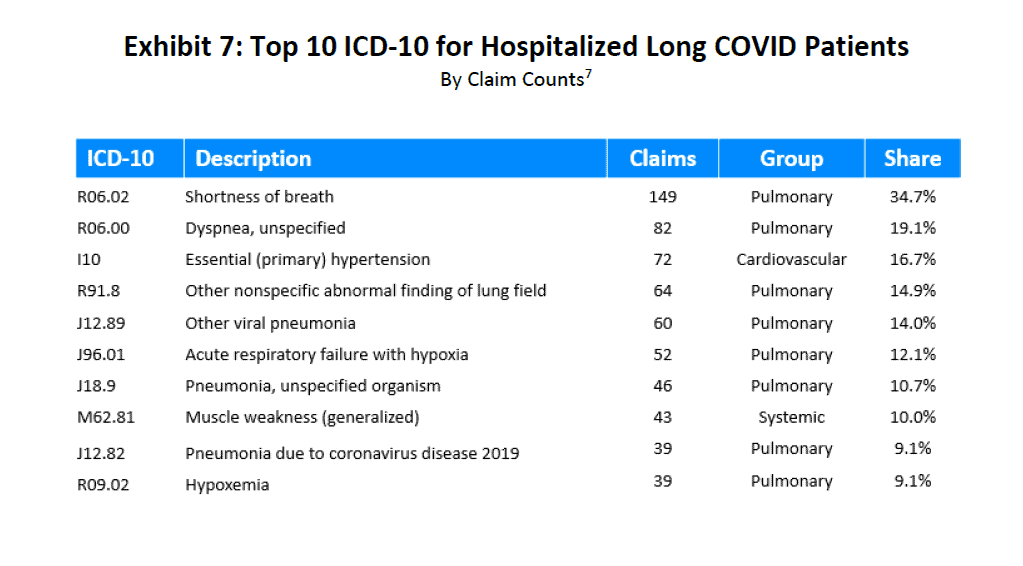
In Exhibits 7 and 8, the two most common diagnosis codes (ICD-10 CM) occurring in each of the hospitalized and nonhospitalized patient cohorts were R06.02 (Shortness of breath) and R06.00 (Dyspnea). Both of these ICD-10 codes are from the pulmonary grouping. Note that for the hospitalized cohort, pulmonary illness dominated the top 10. For the nonhospitalized cohort, Exhibit 8 lists a mix of both pulmonary and cardiovascular groups.
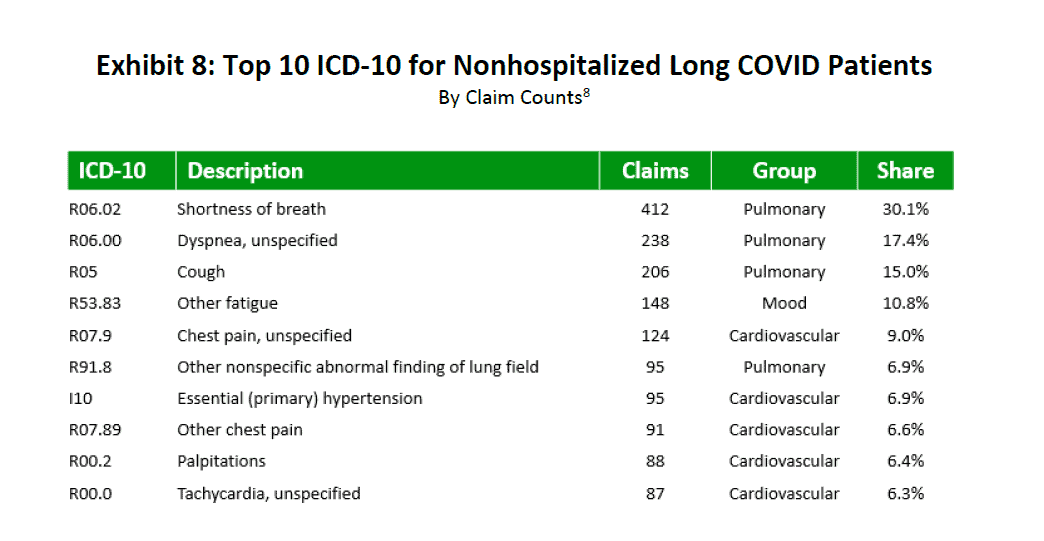
Source: IDC/MDC linking. For each row, the Share column is calculated by dividing the number of claims that include at least the ICD-10 code shown in that row by the total number of hospitalized or nonhospitalized long COVID claims. The rows in the Share column will not total 100% because a single claim can have multiple ICD-10 codes.
7 The number of hospitalized long COVID claims is 430.
8 The number of nonhospitalized long COVID claims is 1,375.
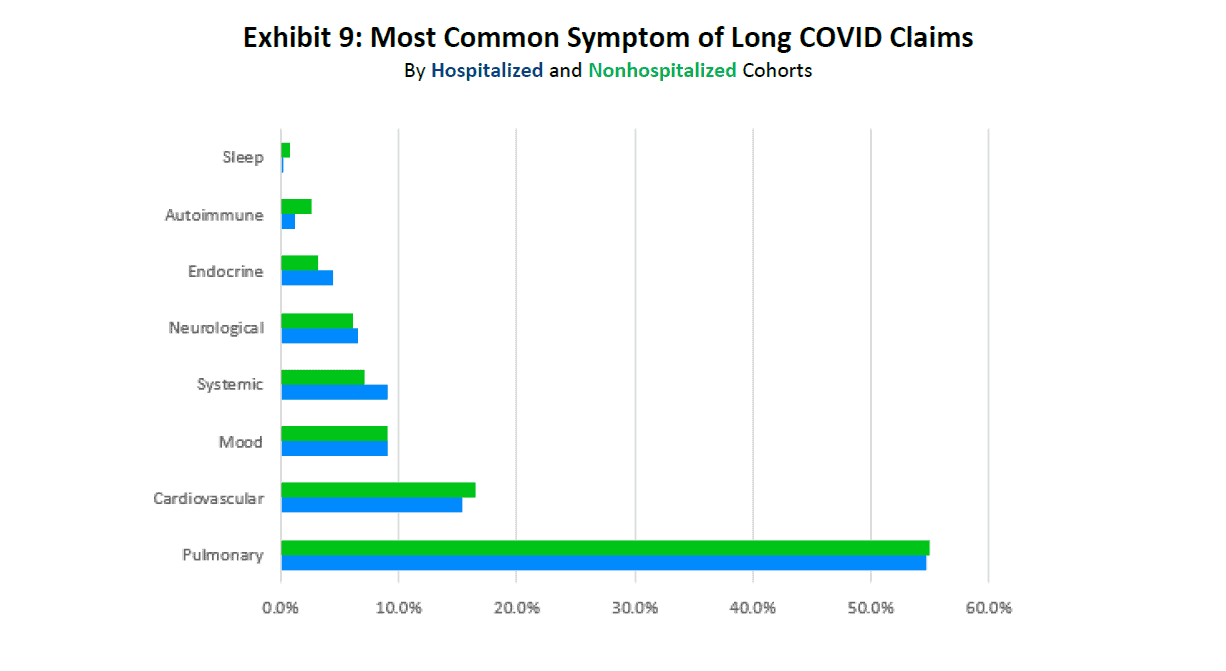
Exhibit 9 shows that COVID-19 claims where pulmonary and cardiovascular symptoms are most common comprised almost 70% of the long COVID claims. Long COVID claims can have symptoms from several long COVID-19 ICD-10 groupings. An assignment to one of eight such groupings is based on which of the symptom groups represents the greatest share of medical payments of the eight during the 30- to 270-day window. The remaining 30% of long COVID claims involved symptoms within the remaining clinical categories related to Mood (e.g., anxiety, depression, and post-traumatic stress disorder), Systemic (e.g., fatigue and weakness), Neurological (e.g., headache, brain fog, and concentration issues), Endocrine (e.g., menstrual issues and thyroid), Autoimmune (e.g., arthralgia and skin), and Sleep dysfunctions. As seen in the exhibit below, the distribution of clinical manifestations of long COVID was very similar between the two study cohorts.
Source: IDC/MDC linking. Claim assignment is based on the maximum medical payment among the eight groups described earlier and observed during the 30- to 270-day window.
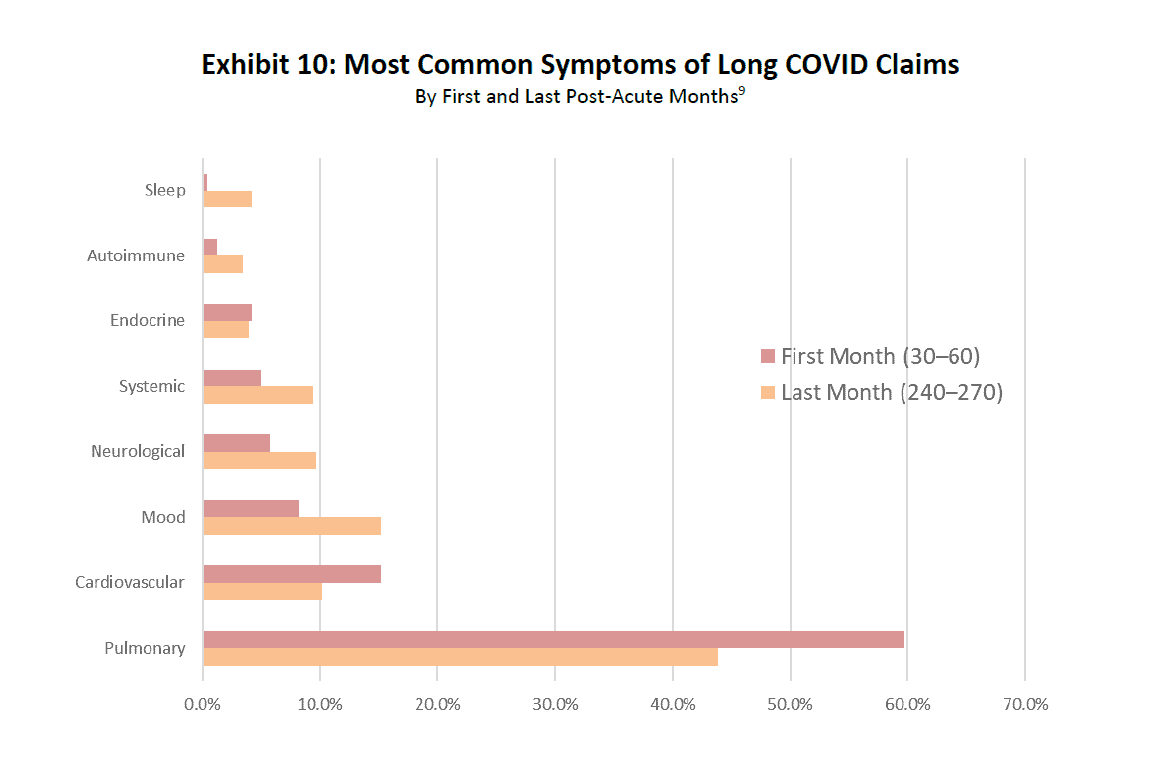
Exhibit 10 examines how symptoms of long COVID evolve over time. Notice the reduction in pulmonary and cardiovascular issues from the first 30 days to the last 30 days. That was offset by an increase in symptoms associated with all other groups, such as Neurological, Mood, Systemic, and Sleep dysfunctions.
Source: IDC/MDC linking.
9 “First month” is defined as greater than 30 days but less than or equal to 60 days from the discharge date for hospitalized patients or from the accident date for nonhospitalized patients. “Last month” is defined as greater than 240 days but less than or equal to 270 days from the discharge date for hospitalized patients or from the accident date for nonhospitalized patients. For the 30- to 60-day window, a long COVID claim is assigned to one of the eight groupings, based on which symptom group represents the greatest share of the medical payments among the eight groupings and made during the 30- to 60-day window. The process is the same for long COVID assignment symptom groups for the 240- to 270-day window.
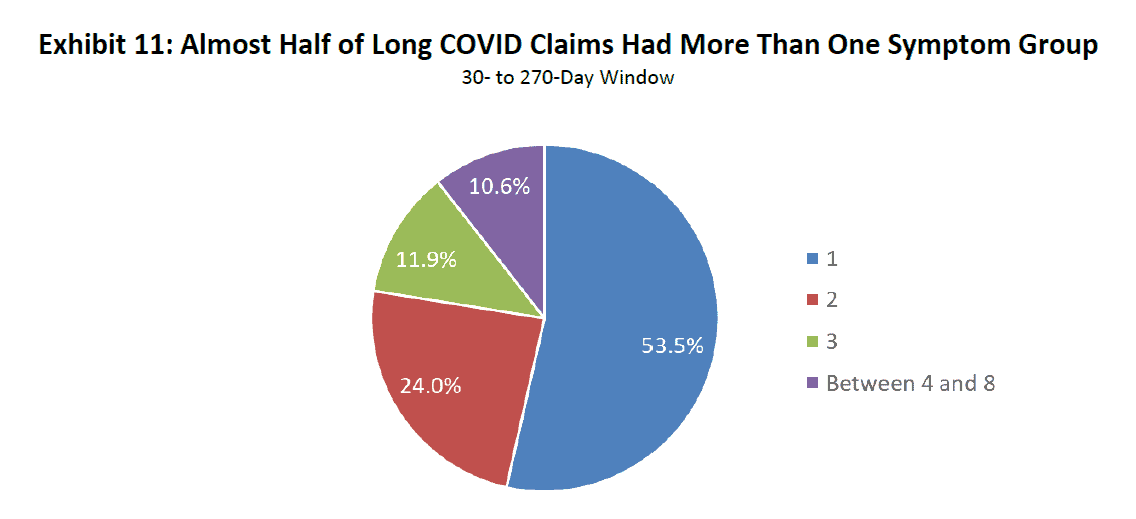
Exhibit 11 shows that nearly half of long COVID patients experienced symptoms from more than one group of symptoms. Claims having symptoms from two groups comprised 24% of claims, while the share of claims with three symptoms was almost 12%. Approximately 1 in 10 claims had symptoms from at least four groupings.
Source: IDC/MDC linking. The number of symptom groups is calculated by examining medical payments associated with the groups. For example, two-symptom groups would include claims with nonzero payments in two of the eight symptom groups.
For patients with long COVID symptoms in more than one symptom group, most have symptoms associated with pulmonary and cardiovascular illnesses.
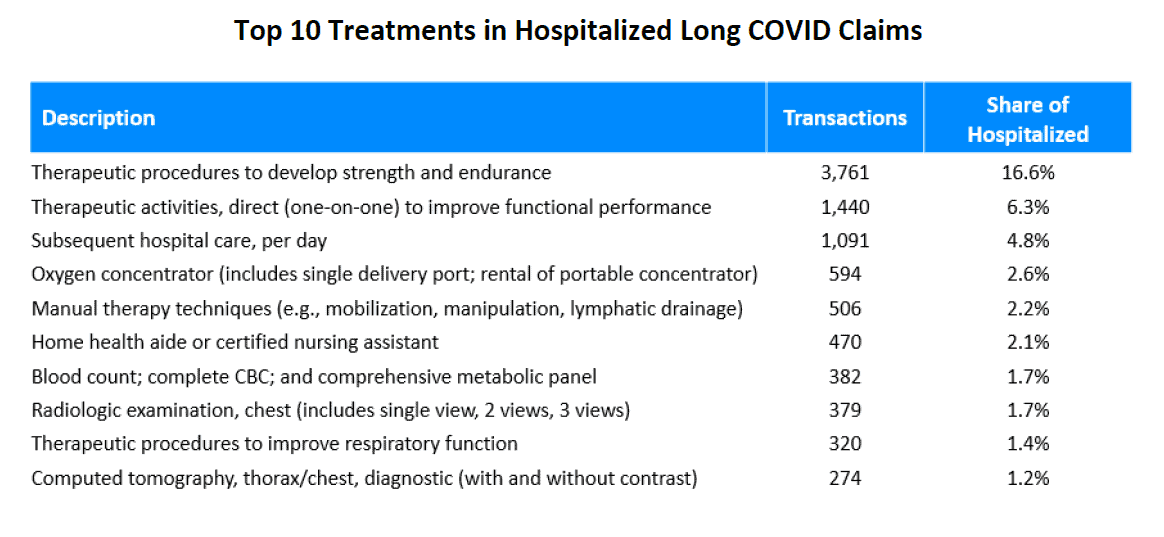
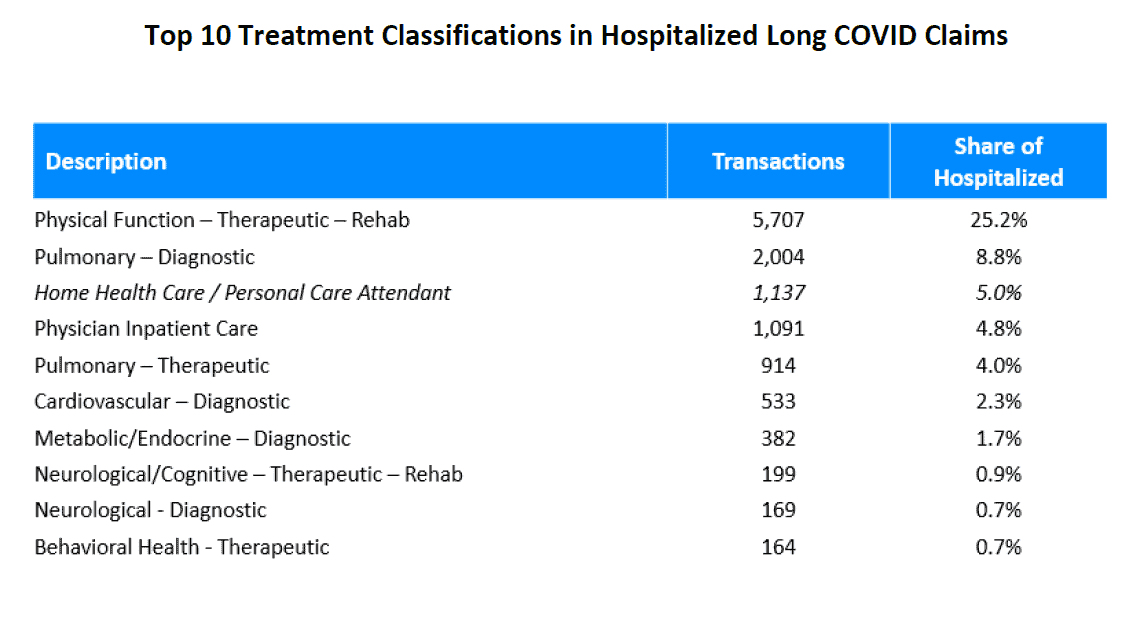
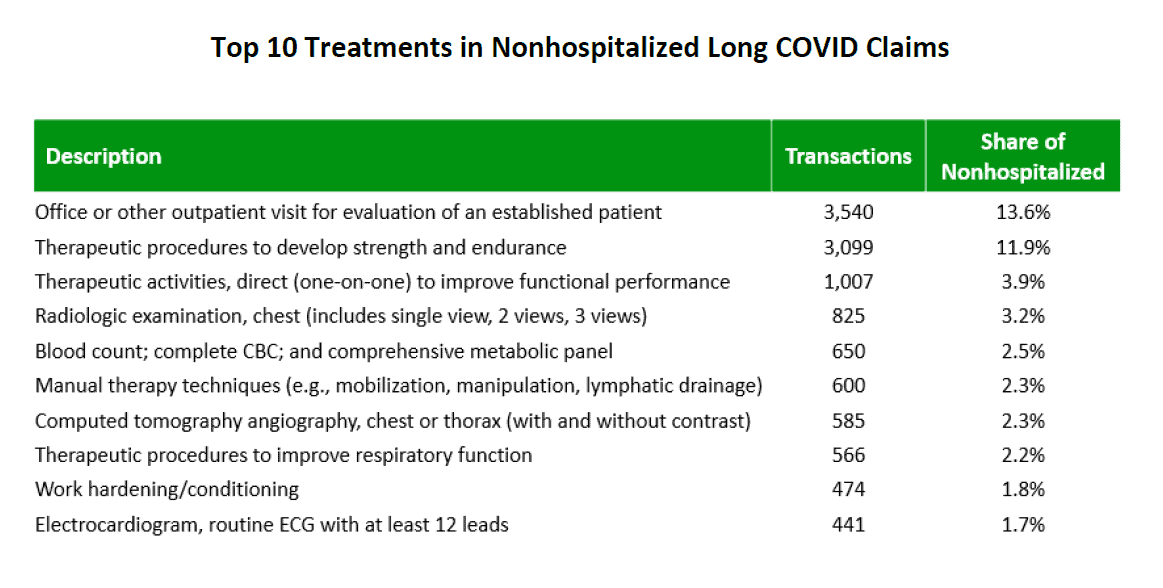
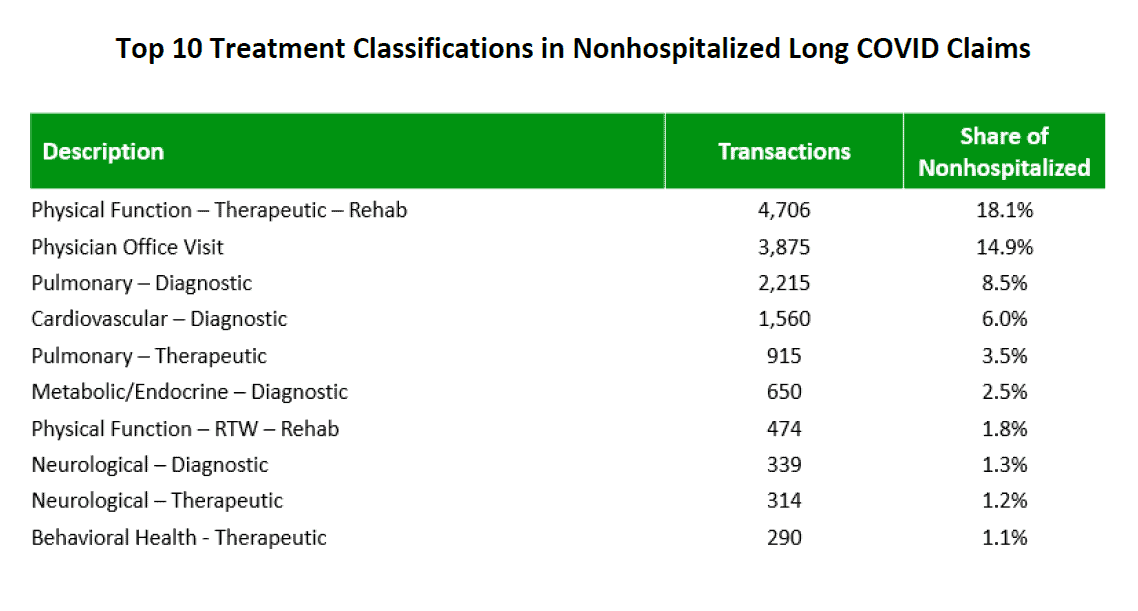
Although the medical community does not entirely understand the pathophysiology or mechanisms behind the clinical symptoms associated with long Covid, there are certain types of medical treatments used more frequently in both cohorts. For example, based on the percentage of transactions, therapeutic procedures to develop strength and endurance are among the top medical treatments for both cohorts. For other top treatments, those that are within the physical function rehabilitation and pulmonary diagnostic categories are most prevalent regardless of hospitalization status. For a list of the top 10 treatments and treatment classifications in each cohort, see Appendix C.
Also noteworthy among the top 10 treatments for the hospitalized cohort is the presence of “oxygen-related treatments” and “treatments provided by home health aides or certified nursing assistants,” which are not among the top 10 of the nonhospitalized cohort. This is not surprising, since hospitalized claims involve more severe illnesses that typically require more oxygen-related support services as well as more home care nursing assistance post-discharge from the hospital.
Given the prevalence of pulmonary and cardiovascular symptoms among both cohorts, the most prescribed drugs include pulmonary inhalers and cardiac drugs, although there are some notable differences between the two cohorts. Most notable is the #2 ranking for steroids for the nonhospitalized cohort, which does not appear among the most prescribed drugs for the hospitalized cohort. One theory for this difference is that, during the earlier stages of the pandemic, steroids were viewed as a frontline therapy for patients who did not require hospitalization and for whom the main goal was to reduce body inflammation. For a list of the top drugs for each cohort, see Appendix C.
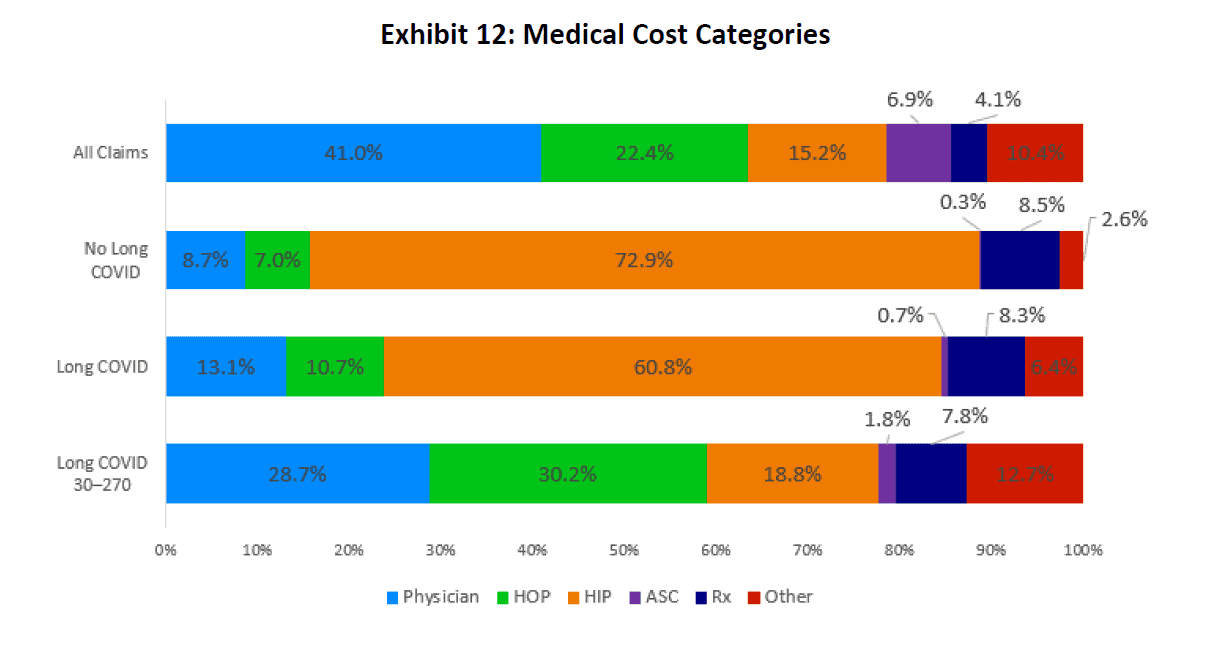
As seen in the middle two bars of Exhibit 12, hospital inpatient (HIP) costs made up most of the medical costs for COVID-19 patients.10 For patients with no long COVID symptoms, 73% of total medical costs were attributed to HIP care. For patients who developed long COVID symptoms, HIP costs comprised 61% of all medical costs. The medical cost distributions for these two cohorts differed markedly from other distributions. Most notably, they differed from the distribution of medical costs for:
- All WC claims (top bar).
- Payments for long COVID patients made in the 30- to 270-day window (bottom bar). That is, once the acute phase of COVID-19 infection ended, the medical distribution was more similar to the distribution for all WC claims.
Source: IDC/MDC linking. All charts include fatal claims.
Medical Cost Category for “All Claims” is based on claims with accident dates from 03/01/2020 to 06/30/2021.
10 Medical costs include payments made during the acute phase as well as during the 30- to 270-day window.
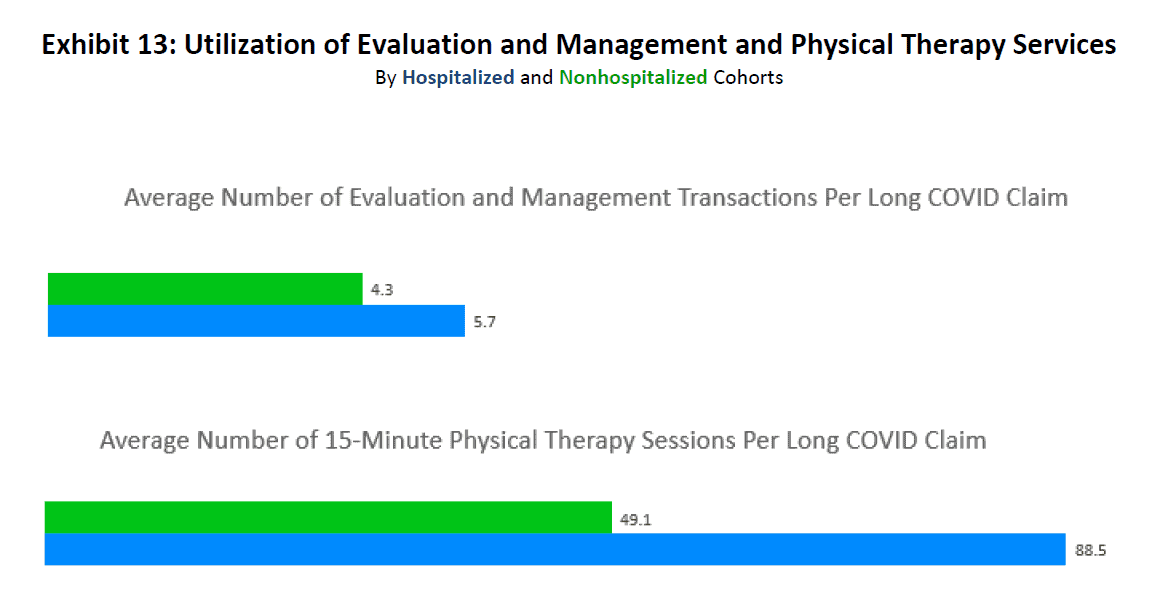
Hospitalized patients are at greater risk of having persistent long COVID symptoms. Of those who were hospitalized, some required prolonged hospitalization and mechanical ventilation. Physical therapists play an important role in assisting with the recovery from long COVID. Exhibit 13 below shows that the average number of 15-minute physical therapy sessions for hospitalized patients who developed long COVID symptoms was almost double the average number of sessions for nonhospitalized patients. It also shows that the hospitalized patients who developed long COVID effects required more visits to their doctors than the nonhospitalized cohort.11
Source: IDC/MDC linking.
11 Regarding measures of statistical significance, the differences in means for both metrics are statistically significant at all common alpha levels.
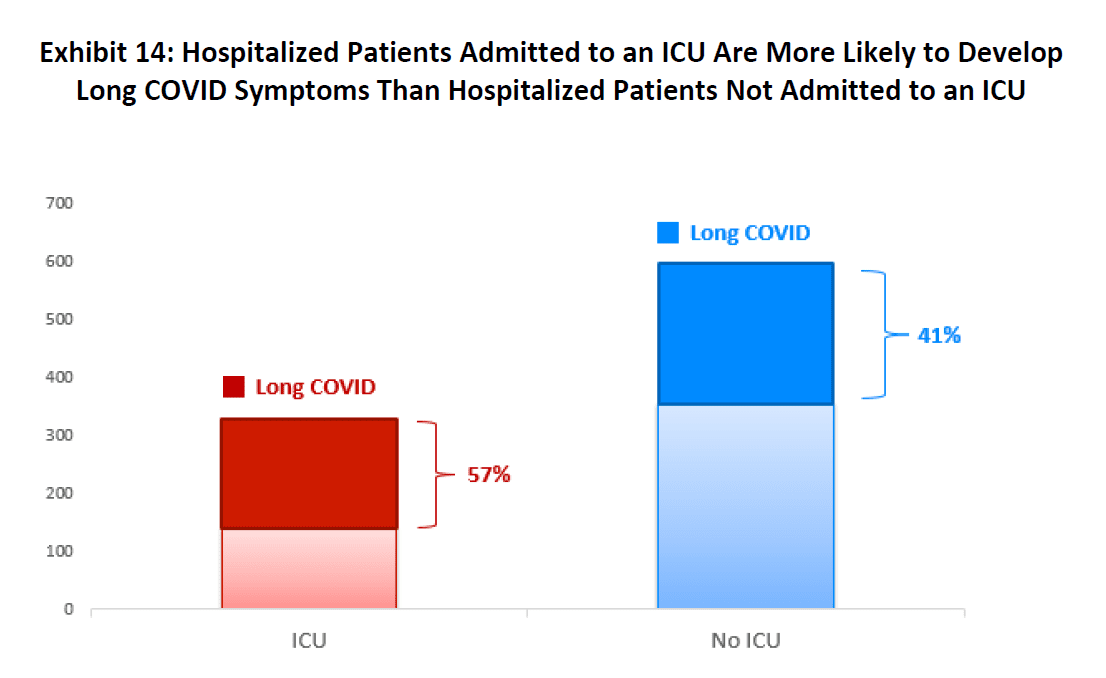
Exhibit 14 below shows that the prevalence of long COVID symptoms was not uniform within the hospitalized cohort. Patients requiring hospitalization that included time in the intensive care unit (ICU) had a 57% chance of developing long COVID symptoms, while the likelihood of long COVID for hospitalized patients without an ICU stay was 41%.12 Furthermore, those who spent time in the ICU had a higher rate of experiencing persistent long COVID symptoms inclusive of clinical manifestations related to post-intensive care syndrome (PICS13). PICS is a collection of dysfunctions involving physical, cognitive, and emotional symptomatology that persist after a patient leaves the ICU. Like long COVID, physical symptoms of PICS may include severe deconditioning with muscle atrophy and weakness, severe generalized fatigue, difficulty breathing from diaphragmatic weakness, anxiety and depression, and cognitive impairments similar to brain fog. Given the limitations of the claims data underlying this research, we are unable to differentiate the long COVID patients from the PICS patients. Nevertheless, it can be presumed that long COVID includes PICS-related symptoms and more likely accounted for the higher rates of symptoms commonly seen in long COVID for those with ICU stays.
Source: IDC/MDC linking.
12 Regarding measures of statistical significance, the difference in likelihoods is statistically significant at all common alpha levels.
13 “Post-intensive Care Syndrome,” Society of Critical Care Medicine, 2013, https://www.sccm.org/MyICUCare/THRIVE/Post-intensive- Care-Syndrome.
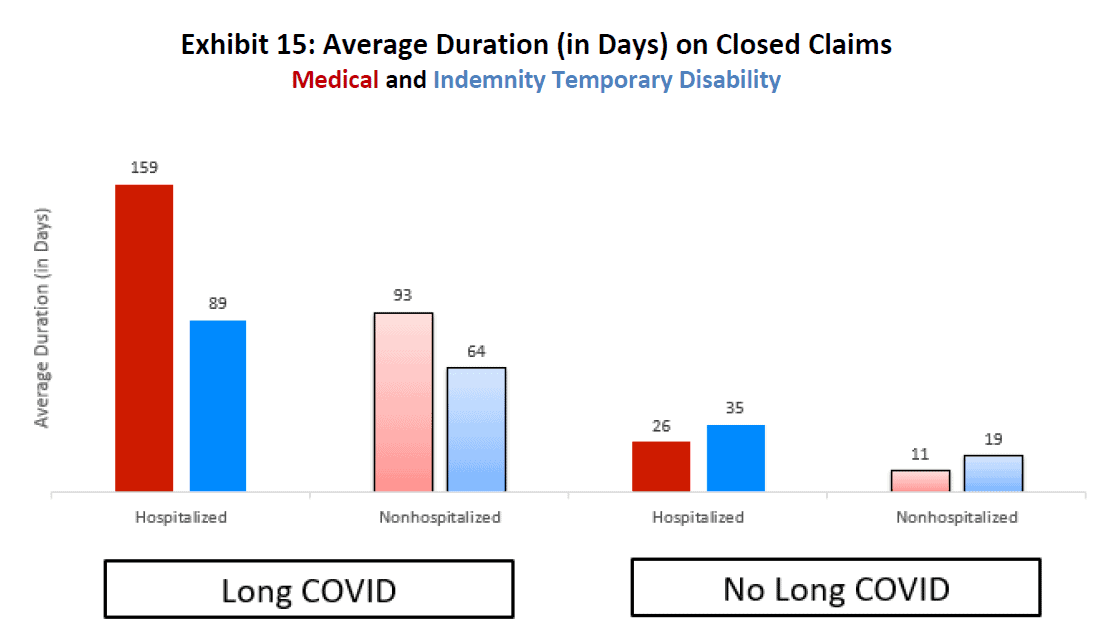
We were interested in learning how long the long COVID condition lasts and the associated benefit payments for that period. Indemnity duration reflects the number of days that the injured worker receives temporary disability benefits.14 Medical duration is measured as the number of days between the first and last medical services rendered.
In Exhibit 15, we observe that, for long COVID claims, the duration of medical treatment was quite a bit longer than the indemnity temporary disability benefit duration. Not surprisingly, the average medical and indemnity durations for the hospitalized long COVID cohort were notably longer than the average durations for the nonhospitalized long COVID cohort. In contrast, those in the “No Long COVID” group had much shorter indemnity benefit and medical treatment durations than those in the “Long COVID” group. What is particularly noteworthy is that, for the “No Long COVID” group, the indemnity benefit duration was longer than the duration of medical treatments for both the hospitalized and nonhospitalized cohorts.
Source: IDC/MDC linking.
14 Indemnity duration excludes any time period when the injured worker was not receiving these benefits, if not paid continuously.
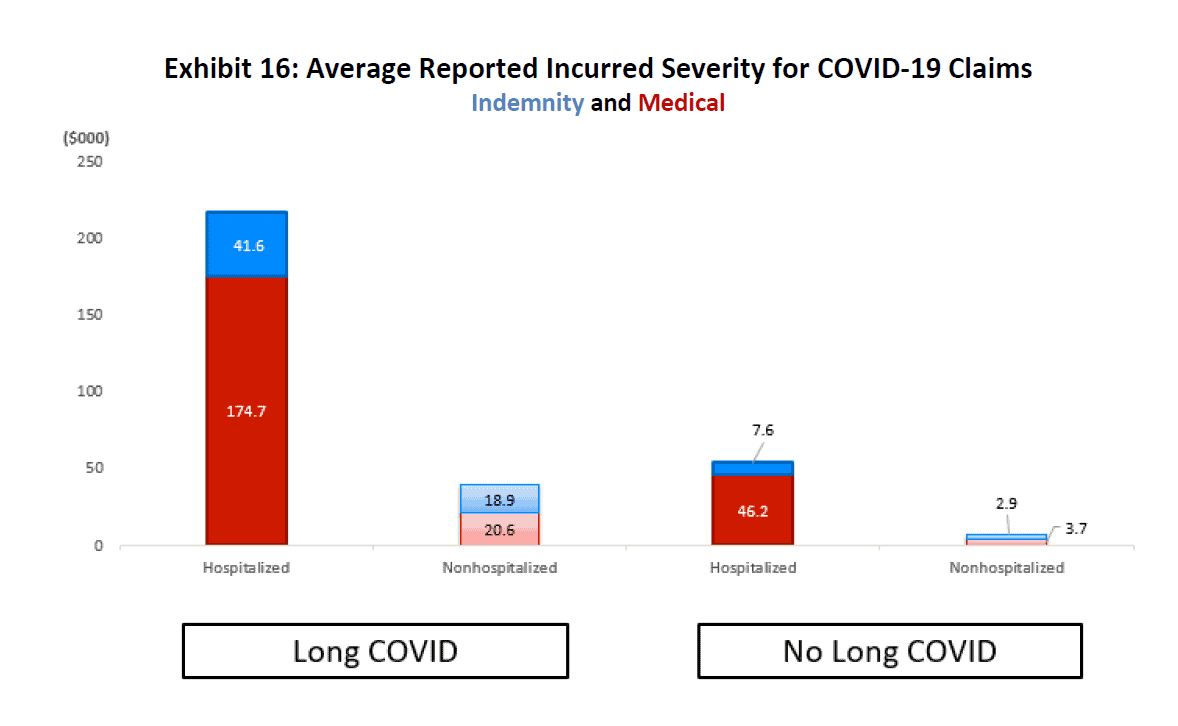
An important characteristic to consider when analyzing the impact of COVID-19 on the WC system is the average cost per claim. Exhibit 16 shows the incurred indemnity, medical, and total claim severities for “Long COVID” and “No Long COVID” claims. Note that these amounts are shown as reported (i.e., no potential development over time is considered).
Total incurred (reported payments plus case reserves) is represented by the height of the bar.
- Hospitalized long COVID claims had the highest severity of any of the cohorts, at just over $216k per claim, with about 80% of total claim costs going toward medical benefits
- Total incurred for nonhospitalized long COVID claims was nearly $40k, roughly split evenly between indemnity and medical
- For hospitalized No Long COVID claims, the incurred severity was just over $53k, with more than 85% going toward medical
- Nonhospitalized No Long COVID claims represented the smallest incurred severity of the various cohorts, at less than $7k per claim
Bottom line: Incurred losses show that claims involving hospitalization were likely to cost significantly more than those that did not require hospitalization.
Source: IDC/MDC linking. Incurred severity is defined as paid losses plus outstanding reserves, and it excludes Incurred but Not Reported (IBNR) reserves.
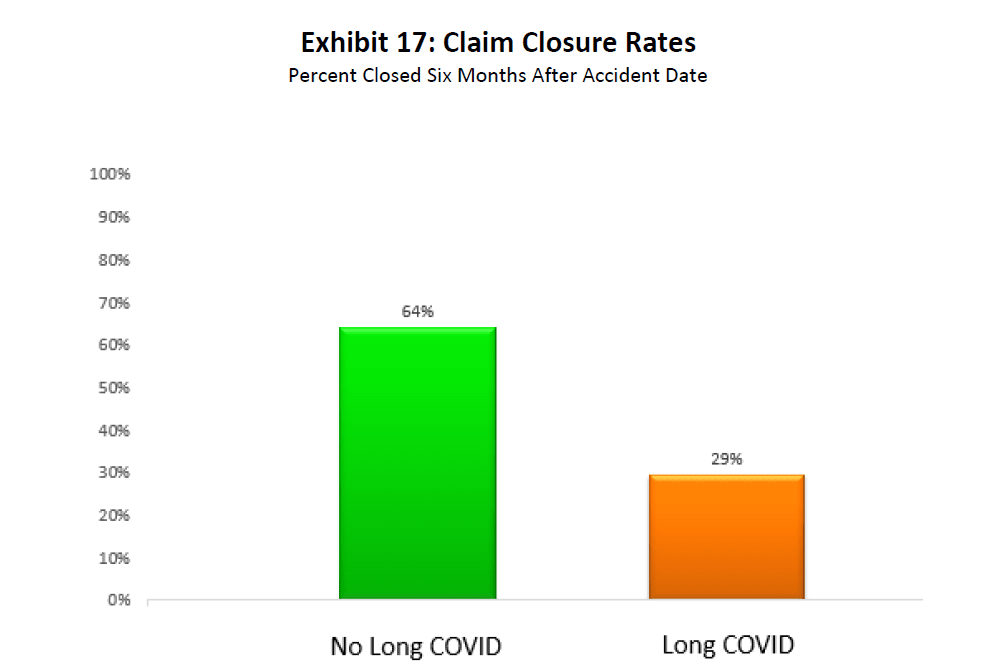
Exhibit 17 compares the claim closure rate between the “No Long COVID” and “Long COVID” cohorts six months after the accident date. Almost two thirds of No Long COVID claims were closed within six months of the accident date. The corresponding share for Long COVID claims was less than half of that (at 29%). The higher rate of claim closures for No Long COVID claims is expected. Because many of these claims did not incur medical treatment for symptoms related to long COVID more than 30 days after discharge or accident date, a lower severity of illness and increased likelihood for claim closure is indicated.
Source: IDC/MDC linking.
Exhibit 18 shows that the share of COVID-19 WC claims for patients who died was about 1%. The average age of such claimants was 61. Exhibit 18 also breaks down the mortality rate into four cohorts: “Hospitalized Long COVID” patients, “Hospitalized No Long COVID” patients, “Nonhospitalized Long Covid” patients, and “Nonhospitalized No Long COVID” patients. Since the Hospitalized No Long COVID cohort consisted of some percentage of seriously ill patients—many of whom may have eventually succumbed to the virus during the initial hospitalization—it is not surprising that the largest share of fatalities among all four cohorts, almost 12%, is observed for that cohort. The share of fatalities among patients discharged from, or never admitted to, the hospital was no more than 0.5%.
Exhibit 18: Fatal COVID-19 Claims
| Cohort | Claims in Cohort | Fatal Claims | % Fatal Within Cohort | |
| Hospitalized | Long COVID | 432 | 2 | 0.5% |
| No Long COVID | 558 | 64 | 11.5% | |
| Nonhospitalized | Long COVID | 1,381 | 6 | 0.4% |
| No Long COVID | 5,369 | 17 | 0.3% | |
| TOTAL | 7,740 | 89 | 1.1% | |
Source: IDC/MDC linking.
CONCLUDING REMARKS
This research brief examined claims for long COVID, a term used to describe presence of various symptoms weeks or even months after the initial contraction of the virus. The symptoms can be continuous or on a relapsing basis. Almost half the hospitalized COVID-19 patients showed at least one symptom related to long COVID after 30 days from the initial hospital discharge date. The rate for the nonhospitalized cohort was 20%. These findings align with other published studies in the sense that there is a high prevalence of continued symptoms months after contracting the virus, which will inevitably cause ramifications for the WC system. Furthermore, NCCI’s COVID claims data related to clinical manifestations and symptom duration corroborate the recently published clinical and epidemiological findings in medical research studies.
Although our initial analysis of long COVID certainly brings to light that long COVID claims are impacting the WC industry, the ultimate consequence or outcome in disability and costs remains uncertain. Since our analysis was limited to the data collected through the first quarter of 2022, the impact of the more infectious or contagious Omicron variant of COVID-19 on long COVID in 2022 also remains unknown at this time. However, we feel encouraged and reassured by the progress that has been made toward prevention and more effective treatments for COVID-19 infections.
ACKNOWLEDGMENTS
The authors would like to thank Barry Lipton, Cary Ginter, and Raji Chadarevian for their review, assistance, and suggested improvements. This research brief was also enhanced by helpful comments and feedback from members of the NCCI Actuarial Committee and the Medical Data Call Research Committee.
REFERENCES
- Groff, Destin, et , “Short-term and Long-term Rates of Postacute Sequelae of SARS-CoV-2 Infection: A Systematic Review” JAMA Network Infectious Disease, October 13 2021 – Doi:10.1001/jamanetworkopen.2021.28568.
- Bull-Otterson, Lara, et , “Post–COVID Conditions Among Adult COVID-19 Survivors Aged 18–64 and ≥65 Years — United States, March 2020–November 2021,” Centers for Disease Control and Prevention, May 2022.
- Crimmins, Eileen , et al., “Differences between Men and Women in Mortality and the Health Dimensions of the Morbidity Process,” Clinical Chemistry, Volume 65, Issue 1, January 2019.
- “Current Cigarette Smoking Among Adults in the United States,” Centers for Disease Control and Prevention, March 17,
2022, https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm.
- Bernacki, Edward , et al., “Attributes of Long Duration COVID-19 Workers’ Compensation Claims,” Journal of Occupational and Environmental Medicine, Volume 64, Issue 5, May 2022.
- Zhang, Julia., et al., “Medical Treatments and Costs of COVID-19 Claims and an Early Look at “‘Long COVID’ in the California Workers’ Compensation System,” Workers’ Compensation Insurance Rating Bureau of California, March
Glossary
ICD-10 Codes: The International Classification of Diseases, Tenth Revision, is a system used by physicians and other health care providers to classify and code all diagnoses, symptoms, and procedures recorded in conjunction with hospital care in the United States.
Indemnity Data Call (IDC): Captures transaction-level detail for indemnity benefit payments, as well as summarized paid and incurred-to-date information on a quarterly basis. It contains the data reported by all WC carriers that write at least 1% of the market share in any one state for which NCCI provides ratemaking services. Some segments of the business may be excluded, and self-insured data is not included. Subject to these conditions, the IDC consists of claims for which an indemnity payment has been made or indemnity reserve established.
International Statistical Classification of Diseases and Related Health Problems (ICD-10): A classification of diseases and other health problems based on a diagnosis maintained by the World Health Organization (WHO).
Medical Data Call: Captures medical transactions reported by all WC carriers that write at least 1% of the market share in any one state for which NCCI provides ratemaking services. Medical transactions are reported for each WC claim until the claim is closed, or until 30 years from the accident date. Lump-sum payments or payments in bulk are not systematically reported, and self-insured data is not included.
Transaction: A line item of a medical bill.
APPENDIX A: ICD-10 CODES ASSOCIATED WITH LONG COVID
| ICD-10 | Long COVID Symptom | ICD-10 Description |
| G93.3 | Systemic | Post-viral fatigue syndrome |
| M35.81 | Systemic | Multisystem inflammatory syndrome |
| M62.81 | Systemic | Muscle weakness (generalized) |
| M79.1 | Systemic | Myalgia |
| M79.7 | Systemic | Fibromyalgia |
| R10 | Systemic | Symptoms and signs involving the digestive system and abdomen |
| R50.81 | Systemic | Fever presenting with conditions classified elsewhere |
| R50.9 | Systemic | Fever, unspecified |
| T73.2XXA | Systemic | Exhaustion due to exposure, initial encounter |
| I10-I16 | Cardiovascular | Hypertensive diseases |
| I26 | Cardiovascular | Pulmonary embolism |
| I34.0 | Cardiovascular | Nonrheumatic mitral (valve) insufficiency |
| I42 | Cardiovascular | Cardiomyopathy |
| I48.0 | Cardiovascular | Paroxysmal atrial fibrillation |
| I48.9 | Cardiovascular | Unspecified atrial fibrillation and atrial flutter |
| I48.3 | Cardiovascular | Typical atrial flutter |
| I49.5 | Cardiovascular | Sick sinus syndrome |
| I49.8 | Cardiovascular | Other specified cardiac arrhythmias |
| I49.9 | Cardiovascular | Cardiac arrhythmia, unspecified |
| I50.2 | Cardiovascular | Systolic (congestive) heart failure |
| I50.3 | Cardiovascular | Diastolic (congestive) heart failure |
| I50.4 | Cardiovascular | Combined systolic (congestive) and diastolic (congestive) heart failure |
| I50.9 | Cardiovascular | Heart failure, unspecified |
| I65.21 | Cardiovascular | Occlusion and stenosis of right carotid artery |
| I87.2 | Cardiovascular | Venous insufficiency (chronic) (peripheral) |
| M05.3 | Cardiovascular | Rheumatoid heart disease with rheumatoid arthritis |
| R00 | Cardiovascular | Abnormalities of heartbeat |
| R07 | Cardiovascular | Pain in throat and chest |
| R55 | Cardiovascular | Syncope and collapse |
| R60 | Cardiovascular | Edema, not elsewhere classified |
| I27.20 | Pulmonary | Pulmonary hypertension, unspecified |
| J00-J99 | Pulmonary | Diseases of the respiratory system |
| M05.1 | Pulmonary | Rheumatoid lung disease with rheumatoid arthritis |
| R05 | Pulmonary | Cough |
| R06 | Pulmonary | Abnormalities of breathing |
| R09.02 | Pulmonary | Hypoxemia |
| R91.8 | Pulmonary | Other nonspecific abnormal finding of lung field |
| S27 | Pulmonary | Injury of other and unspecified intrathoracic organs |
| Z87.01 | Pulmonary | Personal history of pneumonia (recurrent) |
| G31.84 | Neurological | Mild cognitive impairment, so stated |
| G43.009 | Neurological | Migraine without aura, not intractable, without status migrainosus |
| G43.019 | Neurological | Migraine without aura, intractable, without status migrainosus |
| G43.109 | Neurological | Migraine with aura, not intractable, without status migrainosus |
| G43.809 | Neurological | Other migraine, not intractable, without status migrainosus |
| G43.811 | Neurological | Other migraine, intractable, with status migrainosus |
| G43.909 | Neurological | Migraine, unspecified, not intractable, without status migrainosus |
| G44.001 | Neurological | Cluster headache syndrome, unspecified, intractable |
| G44.52 | Neurological | New daily persistent headache (NDPH) |
| G44.85 | Neurological | Primary stabbing headache |
| G44.89 | Neurological | Other headache syndrome |
| G51.0 | Neurological | Bell’s palsy |
| G56.0 | Neurological | Carpal tunnel syndrome |
| G58.9 | Neurological | Mononeuropathy, unspecified |
| G60.3 | Neurological | Idiopathic progressive neuropathy |
| G61.0 | Neurological | Guillain-Barré syndrome |
| G61.81 | Neurological | Chronic inflammatory demyelinating polyneuritis |
| G62.8 | Neurological | Other specified polyneuropathies |
| G72.81 | Neurological | Critical illness myopathy |
| G93.1 | Neurological | Anoxic brain damage, not elsewhere classified |
| G93.4 | Neurological | Other and unspecified encephalopathy |
| G93.89 | Neurological | Other specified disorders of the brain |
| H49.20 | Neurological | Sixth [abducent] nerve palsy, unspecified eye |
| H53.9 | Neurological | Unspecified visual disturbance |
| H53.19 | Neurological | Other subjective visual disturbances |
| H53.2 | Neurological | Diplopia |
| H53.30 | Neurological | Unspecified disorder of binocular vision |
| H53.8 | Neurological | Other visual disturbances |
| H81.1 | Neurological | Benign paroxysmal vertigo |
| H81.2 | Neurological | Vestibular neuronitis |
| H81.39 | Neurological | Other peripheral vertigo |
| H81.8X | Neurological | Other disorders of vestibular function |
| H81.9 | Neurological | Unspecified disorder of vestibular function |
| H90.3 | Neurological | Sensorineural hearing loss, bilateral |
| I63.30 | Neurological | Cerebral infarction due to thrombosis of unspecified cerebral artery |
| I63.9 | Neurological | Cerebral infarction, unspecified |
| M79.2 | Neurological | Neuralgia and neuritis, unspecified |
| M99.00 | Neurological | Segmental and somatic dysfunction of head region |
| R20.1 | Neurological | Hypoesthesia of skin |
| R20.2 | Neurological | Paresthesia of skin |
| R27.9 | Neurological | Unspecified lack of coordination |
| R41.0 | Neurological | Disorientation, unspecified |
| R41.840 | Neurological | Attention and concentration deficit |
| R41.841 | Neurological | Cognitive communication deficit |
| R41.89 | Neurological | Other symptoms and signs involving cognitive functions and awareness |
| R41.9 | Neurological | Unspecified symptoms and signs involving cognitive functions and awareness |
| R42 | Neurological | Dizziness and giddiness |
| R43 | Neurological | Disturbances of smell and taste |
| R47.01 | Neurological | Aphasia |
| R47.81 | Neurological | Slurred speech |
| R47.89 | Neurological | Other speech disturbances |
| R47.9 | Neurological | Unspecified speech disturbances |
| R51 | Neurological | Headache |
| R56.9 | Neurological | Unspecified convulsions |
| R90.89 | Neurological | Other abnormal findings on diagnostic imaging of central nervous system |
| S24 | Neurological | Injury of nerves and spinal cord at thorax level |
| E00-E99 | Endocrine | Endocrine, nutritional, and metabolic diseases |
| N92 | Endocrine | Excessive, frequent, and irregular menstruation |
| R63.4 | Endocrine | Abnormal weight loss |
| R63.5 | Endocrine | Abnormal weight gain |
| S19.84 | Endocrine | Other specified injuries of thyroid gland |
| M05.5 | Autoimmune | Rheumatoid polyneuropathy with rheumatoid arthritis |
| M25.40 | Autoimmune | Effusion, unspecified joint |
| M25.5 | Autoimmune | Pain in joint |
| M25.6 | Autoimmune | Stiffness of joint, not elsewhere classified |
| R21 | Autoimmune | Rash and other nonspecific skin eruption |
| F06 | Mood | Other mental disorders due to known physiological condition |
| F30 | Mood | Manic episode |
| F32 | Mood | Depressive episode |
| F33 | Mood | Major depressive disorder, recurrent |
| F34 | Mood | Persistent mood [affective] disorders |
| F39 | Mood | Unspecified mood [affective] disorder |
| F40-F48 | Mood | Anxiety, dissociative, stress-related, somatoform and other nonpsychotic mental disorders |
| R53 | Mood | Malaise and fatigue |
| F51 | Sleep | Sleep disorders not due to a substance or known physiological condition |
| G47 | Sleep | Sleep disorders |
| Z72.82 | Sleep | Problems related to sleep |
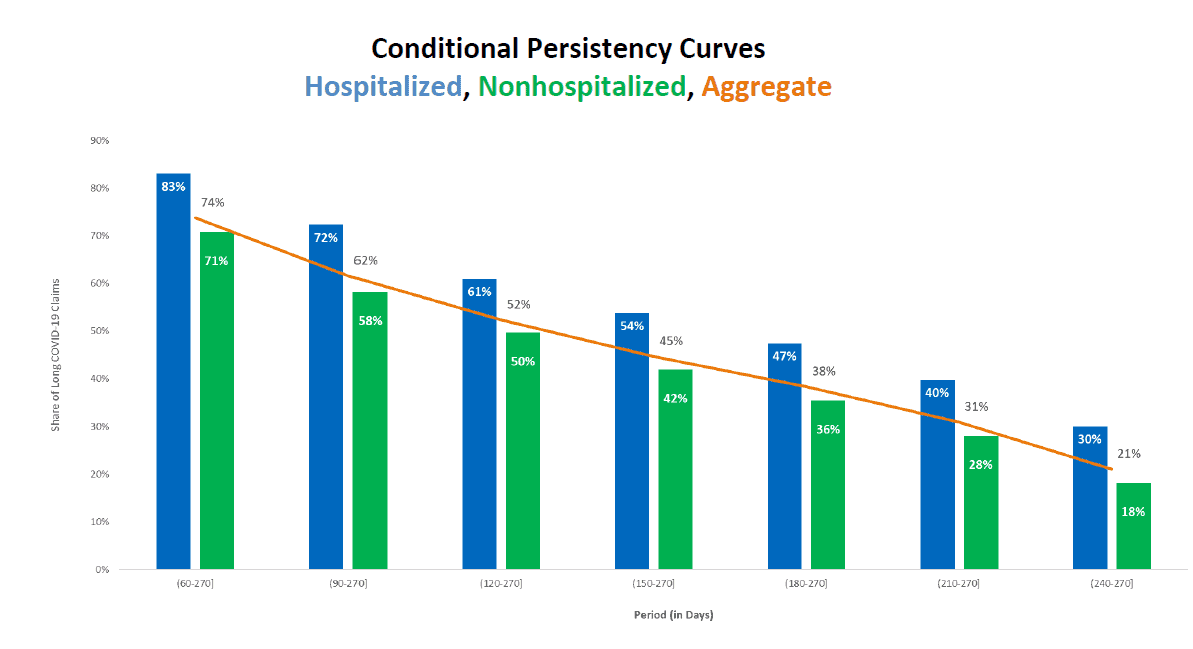
APPENDIX B: PERSISTENCY CURVE
Persistency curves help us answer yet another question: For long COVID claims, what is the likelihood that such patients will continue to have long COVID symptoms in the future?
To help answer this question, we use conditional persistency curves as shown below. The first point in the graph below, labeled as (60, 270], shows that 83% of patients who were hospitalized and showing at least one long COVID symptom beyond 30 days continued to show long COVID symptoms beyond 60 days. For the nonhospitalized cohort, the corresponding figure was somewhat lower, at 71%.15
Overall, this exhibit indicates that patients who were hospitalized and developed at least one long COVID symptom beyond 30 days were more likely to continue having health issues post COVID than nonhospitalized patients.
APPENDIX C: TOP TREATMENTS AND TREATMENT CLASSIFICATIONS ASSOCIATED WITH LONG COVID
Source: IDC/MDC linking.
Source: IDC/MDC linking.
Source: IDC/MDC linking.
ABOUT THE AUTHORS
Robert Moss joined NCCI in 2002 and works in the actuarial ratemaking and legislative analysis and research areas. He is an Associate of the Casualty Actuarial Society and a Member of the American Academy of Actuaries.
Nedžad Arnautović joined NCCI in 2013 and works in the actuarial research area. He is an Associate of the Casualty Actuarial Society.
Dr. Michael Choo has been Chief Medical Officer and Senior Vice President for Paradigm since January 2013. He is responsible for Paradigm’s physician networks, centers of excellence, outcomes R&D, and medical innovations analysis. Dr. Choo is an emergency medicine instructor at Wright State University’s Boonshoft School of Medicine, senior oral board examiner for American Board of Emergency Medicine, and a former hospital CEO for Regional Care Hospital Partners.
ABOUT PARADIGM
Paradigm is an accountable care management organization focused on improving the lives of people with complex and catastrophic injuries and diagnoses. The company has been a pioneer in value-based care since 1991, offering deep clinical expertise, high-value specialty networks, behavioral health support, payment integrity solutions, and robust data analytics to generate the very best outcomes for patients, payers, and providers.
Paradigm is headquartered in Walnut Creek, California, with offices across the U.S. For more information, please visit www.paradigmcorp.com.
This article is provided solely as a reference tool to be used for informational purposes only. The information in this article shall not be construed or interpreted as providing legal or any other advice. Use of this article for any purpose other than as set forth herein is strictly prohibited. The views and opinions expressed in this article by authors from outside of NCCI are solely those of the author, and do not necessarily reflect the views or opinions of NCCI.