Article originally published in On the Frontline Magazine
An injury or illness arising out of one’s work can be costly. For claimants and their employers, a complete recovery and return to work, as quickly as possible, are ideal, but how do we ensure this happens? The answer lies in medical management programs.
Historically, the longer a workers’ compensation or employers’ liability claim remains open, the greater its expense. As occupational health care costs rise, employers and health care payers want to contain expenses.
“Medical management programs enable early engagement on a claim and a faster return to work, which is good for both the employer and the employee. It’s a win-win for everybody,” says Danielle Lisenbey, president and chief executive officer of Broadspire, a Crawford company.
In medical management, the aim is to get the patient on the right track. This involves a combination of the right price, care coordination and optimizing outcomes. Broadspire also encourages employers to have a return-to-work plan in place, with senior management support, and clear responsibilities for the injured worker and employer.
Click Link to Access Free PDF Download
“The 6-Step Process To Determine Workers’ Comp Injury Causation”
“Medical management is not about securing the cheapest care; it’s about securing the most appropriate care,” said Jim Andrews, executive vice president of prescription benefit management services at Healthcare Solutions, an Optum company. The company, which provides data and care management services to Broadspire, focuses on improving care coordination, which ultimately produces better outcomes at less cost.
“Care coordination is a problem, especially in workers’ compensation. If you can coordinate care in a workers’ compensation claim, you can reduce the redundancy of services,” he says. “It’s a win for the employer because they get the injured workers back to work sooner.”
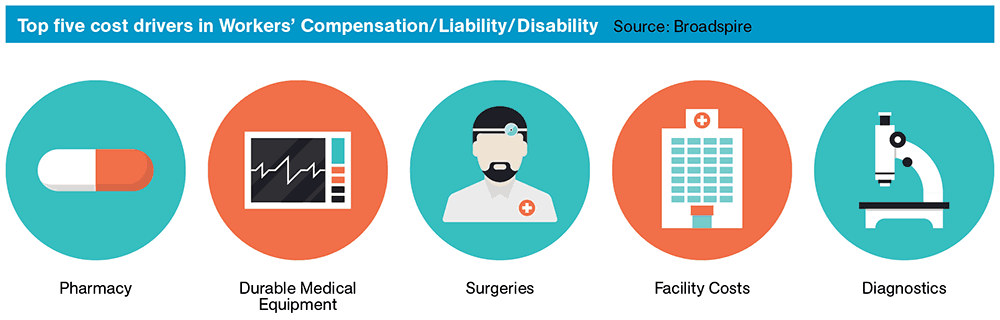
In workers’ compensation claims especially, medical management is an effective way to contain costs. “The medical component is becoming the dominant factor in a workers comp claim,” explains Paul Braun, managing director at Aon Risk Solutions. “From a concentration standpoint, it used to be that about 70% of the claim was for indemnity, and 30% was for medical. Now, it’s almost reversed.”
There has been a significant rise in medical costs over the past decade. Currently, U.S. healthcare spending is on track to hit $10,000 per person or $3.207 trillion in total in 2015, according to a Forbes report. “With the rise in medical costs, there has been a greater focus and need for medical management in all aspects of claims,” says Lisenbey.
“Claimants often are confronted with a lot of different information, from their doctors as well as employers,” she continues. “We help them understand what’s going on with their case, we engage them at the family level and help them understand what questions to ask in order to get the right care.”
Joining the Dots
Medical management services also deliver advanced analytics to employers, Lisenbey notes. Broadspire uses e-triage, a detailed interview process that captures claimant information including co-morbidities that might not be observable. “For example, the e-triage process might reveal that a claimant has a smoking habit, and medical evidence shows that smokers take longer to heal from injuries,” she explains.
That kind of data can help in applying different strategies to further improve the outcome. Similarly, provider analytics enable employers to maximize their physician networks by comparing factors such as durations and costs related to services the physicians provide.
Another tool that Broadspire utilizes is the ‘virtual peer’, a composite of data points that enables comparisons of employers’ experiences and claims trends, even among organizations in different industries. Data that is helping produce better outcomes also involves prescription drugs – one of the fastest-growing components of medical claim costs.
Danielle Lisenbey, President and CEO, Broadspire®
“Our data is available in almost real time, which means it becomes available for analysis in near real time,” says Healthcare Solutions’ Andrews. “Paper-based medical bills take much longer to receive and analyze. Although data analysis on prescriptions can quickly show trends, “it doesn’t always mean that you can do something about it immediately.”
Worrisome drug-related trends in workers’ compensation include: physician dispensing, increasing use of compound pharmaceuticals and use of narcotics to relieve pain. “With narcotics and opioids, it’s important to manage those from an injury and recovery standpoint. You need to offer other services to help people with intractable pain. You can’t just say no to the drugs without offering something else, or coordinating care with the primary physician,” says Andrews.
Modern Day Nursing
Broadspire’s senior nurse reviewer (SNR) program has also driven significant savings since its launch in 2005. It reviews cases and determines an appropriate medical management intervention, with periodic review until a favorable outcome is reached. Among its benefits are: an average reduction in claim payments exceeding 10%, improved closure rates, and reduced litigation rates.
“In workers’ compensation, a cost-saving factor is a return-to-work program,” Aon Risk Solutions’ Braun says. “Return to work is critical, and getting someone like a nurse case manager to assist and support that model is very important.”
In the UK, Broadspire provides medical management services that help employers and claimants navigate the single-payer National Health Service. “The NHS is the first port of call for anyone who’s injured, and hospital and point-of-service medical treatment is covered,” says Deborah Edwards, head of rehabilitation at Broadspire.
“As patients progress through the NHS, the rehabilitation and recovery process becomes patchier,” she continues. “If someone is out of work, they might be waiting six months for surgery in the NHS that could be performed in a week if privately paid. We juggle those services with the goal of rapid return to work.”

Danielle Lisenbey became chief executive officer of Broadspire in 2012. Immediately prior to this role, she was chief operating officer for Medical Services, responsible for the operation of all of Broadspire’s medical and case management services. In this position, she drove the continued development and delivery of products and services that have generated cost containment results typically 10 to 15 percent better than those produced by other TPAs and medical management companies.
During her tenure as chief operating officer, many new service offerings were developed, including: the BOLD® Network, a unique, state-stratified, multi-tiered approach to a preferred provider organization (PPO) strategy; a durable medical equipment (DME) formulary that applies the cost management principles of a pharmacy formulary to medical equipment; and a new chronic pain protocol, a multidisciplinary approach to addressing the complex chronic pain conditions that drive the duration of workers compensation and disability claims.