Authors: Vicki J. Missar, Michael Fray, Candy Raphan, Mary Matz, Wendy Weaver
Whitepaper originally published by The Association of Safe Patient Handling Professionals (ASPHP). All of the authors of this white paper are members in good standing with ASPHP and serve as Board members.
Reference: https://www.choosebroadspire.com/media/11899/safe-patient-handling-white-paper.pdf
Abstract
Healthcare organizations are now engaged in Delivery System Transformation (DST), whereby performance-based incentive payment programs are used to support and reward hospitals for investing in projects that advance care and population health while lowering costs. In these efforts, it becomes critical to understand causes of patient handling and mobility workers’ compensation injury claims. Until now, programs that are self-administered or utilize a Third Party Administrator (TPA) have differing, if any, codes to determine employee injury trends. Unfortunately, these coding structures, particularly when it comes to causes, lack any real, actionable data to establish investment needs for safe patient handling interventions. Healthcare organizations are left to drill down to the accident-description level and extract key causes of the patient handling injury, a time-consuming and unrealistic option given the human resources demand within healthcare. This paper proposes a condensed, yet powerful, sub-level coding structure for safe patient handling claims that any claims reporting system can easily adopt. As a result, this coding structure will eliminate the need to manually sort through lines and lines of data for relevant trends. Adopting this proposed coding structure nationally will reward the safe patient handling community with a consistent and transparent approach to claims. As a result, it will enable facility-level comparison of key functions and tasks associated with patient handling claims, peer-to-peer benchmarking of these causes and return on investment calculations at the fingertips of the end user.
Introduction
Healthcare companies in today’s business environment experience an unprecedented amount of change in terms of change drivers and pace of change: technology, shifting workforce demographics, global opportunity and competition, new sources of competitive advantage and rapidly evolving risk and regulatory requirements. Healthcare is an industry in the midst of fundamental transformation across the entire value chain and to all sectors, including physician groups, individual hospitals, senior care facilities, managed care organizations, insurance companies, wellness organizations, and integrated healthcare systems. As organizations address new business realities driven by healthcare reform and DST, they must reassess their data-mining capabilities around leading loss drivers that impact employee health and safety. With the right data and trending capabilities, safe patient handling claims can be easily dissected and solutions funded.
An apparent need exists to develop a standardized coding method focusing on the sub-category of activity type associated with patient handling injuries. So far, no national standard addresses the way these claims are coded in a Risk Management Information System (RMIS). This lack of uniformity leads to time-consuming efforts to extract key trending and cause analysis for meaningful solutions.
Click Link to Access Free PDF Download
“The 6-Step Process To Determine Workers’ Comp Injury Causation”
Standardization is applicable to overall workers’ compensation management, as well as risk managers, safety practitioners and occupational health professionals concerned with preventing safe patient handling and mobility (SPHM) injuries. The current mechanism to track injury types and occurrences proves neither healthcare specific nor customized by individual stakeholders. In addition, there’s a lack of detail-level standardization to provide easily identifiable and actionable data. Table 1 shows a snapshot of a healthcare organization RMIS loss run. The vague nature of the injury and cause descriptions provide little intelligence on the tasks (e.g. transfer type, toileting, bathing, etc.) performed at the time of injury. Therefore, a significant blind spot remains for safe patient handling professionals, and need for improvement on a national level is evident.
Table 1: Snapshot of a RMIS Loss Run for a Healthcare Organization
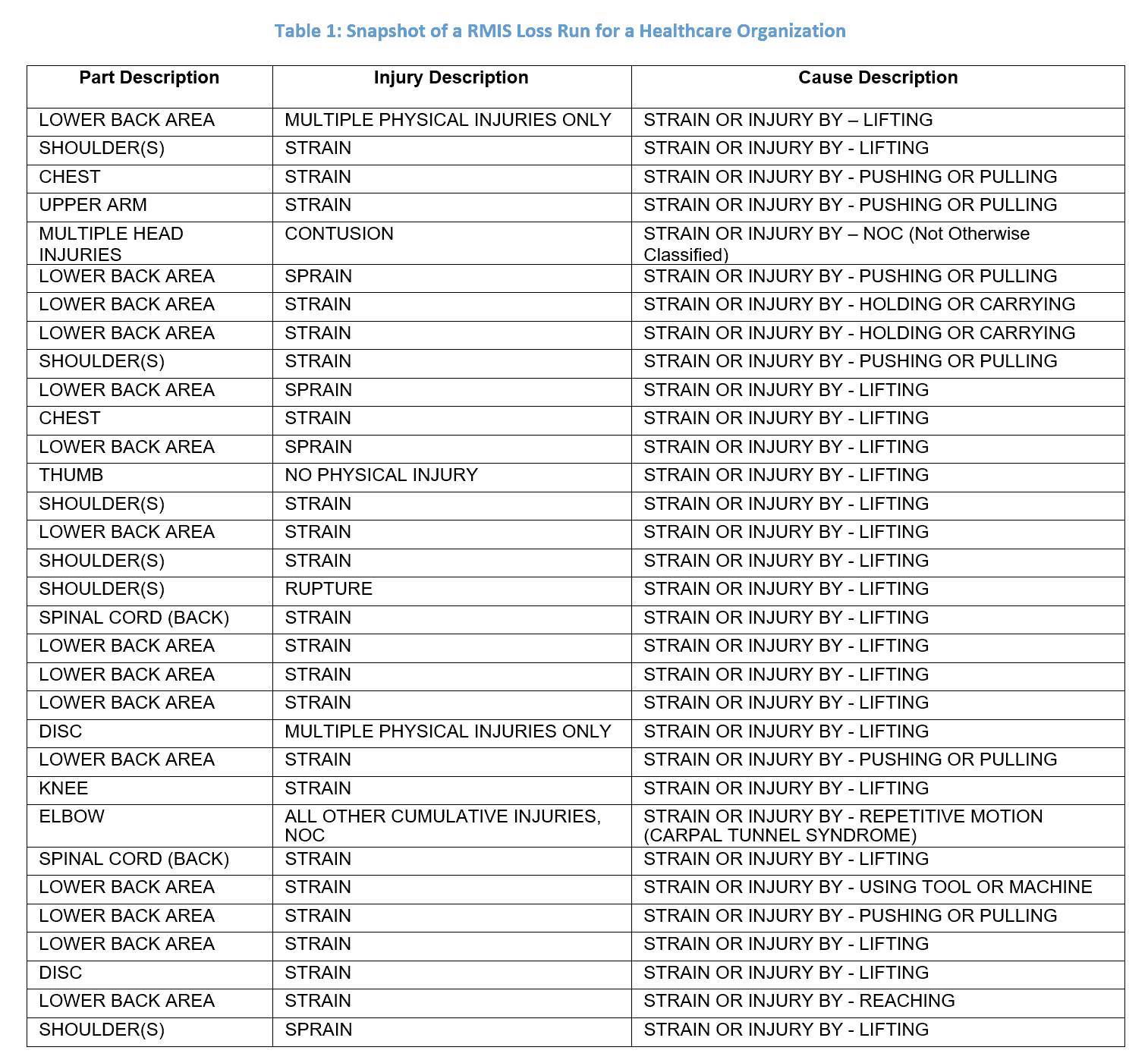
Current State: The Era of Big Data
Claims administrators require the ability to pare down injuries to focus on cost and frequency. Data available through loss run or other high-level data output provide only a general understanding of cause (See Table 1). The table does not provide sufficient detail to describe how the action being performed caused the injury. Technology is available via RMIS to affect change, but it cannot be used productively without changing and improving the information captured. A small addition to the current coding will make patient handling claims/injuries more transparent and actionable, create a best practice in the industry and produce long-lasting benefits.
Multiple methods are used in an attempt to address the need for this transparency which will bring patient handling claim trends forward. The following are examples:
- Manually reviewing narrative reports to ascertain cause, associated circumstances and activities performed at the time of injury
- Creating manual methods to map injuries with specific sites within a facility
- Manually creating and using customized codes specific for a healthcare system or facility
- Benchmarking national research reports that take years to publish
- Using the National Institute for Occupational Safety and Health (NIOSH) Occupational Health Safety Network (OSHN) coding system (NIOSH, 2015)
Manual attempts at transparency are generally labor-intensive and may be highly burdensome. In an environment where human resources are stretched and patient and staff safety have become national priorities, the current state requires change.
Patient Handling Claims
Frequent injuries to patients and residents—regardless of the healthcare setting—have created a national call for action as demonstrated by several laws passed over the past few years. In addition, the American Nursing Association has issued an interprofessional national standard with the goal to put an end to these life-altering and career-ending injuries. The Occupational Safety and Health Administration (OSHA) points to manual patient handling as the cause of the high incidence, and severity, of injuries in the healthcare industry (OSHA, 2003). In 2013, the most frequent national, nonfatal occupational injury and illness, as well as injury and illness requiring days away from work, transfer, or light duty, were within healthcare and social assistance categories (Bureau of Labor Statistics (BLS), 2014). BLS data for 2013 demonstrate this impact on caregivers. As seen in Figure 1, nursing assistants and orderlies accounted for some of the highest rates of nonfatal injuries and illnesses resulting in lost work days. These rates are approximately three times that of construction laborers and similar to that of firefighters. Compounding the personal and organizational impacts of such severe injuries, the financial cost of these injuries is profound (Institute of Medicine, 2011).
Figure 1: BLS Musculoskeletal Injury Rates for 2013 (per 10,000 work hours)
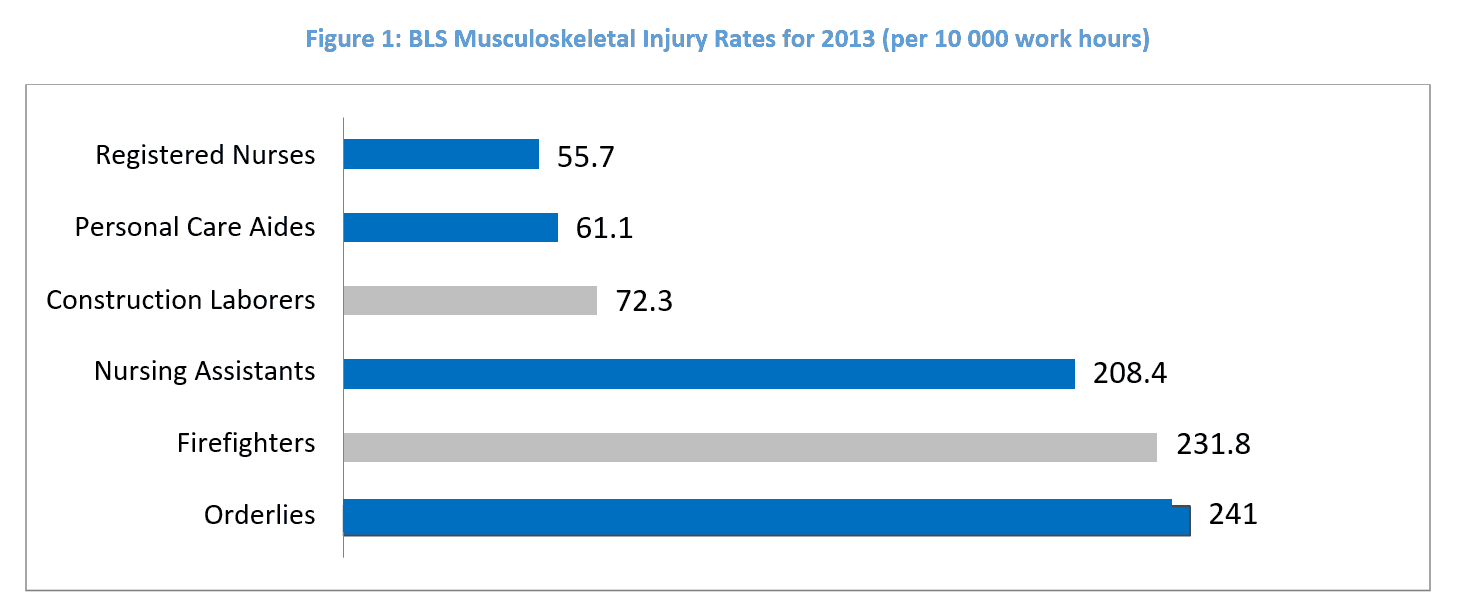
As illustrated above, injuries to caregivers, who are providing essential services for the infirm, are clearly significant. A typical certified nursing assistant, one who provides the majority of direct patient care, averages 4.5 injuries per year, according to a study by Khatutsky et.al (2012). However, while the study listed patient handling as a key loss driver, the study did not define the cause or activity (toileting, repositioning, etc.) involved in the injuries. Lack of easily accessed injury details on a sub-category level is a significant disadvantage for many SPHM professionals. Without that detail, there is no mechanism to facilitate implementation of effective Safe Patient Handling and Mobility Programs using RMIS data. Practitioners are left with manual, time- consuming data-crunching processes.
Reaffirming the Core Problem
There is a significant lack of easily accessible, detailed causative factors related to patient handling and mobility incidents available to healthcare sectors and stakeholders on a cumulative level. Patient handling and mobility incident causality data is generally a labor-intensive extraction effort using manual processes Without key elements, justification for the financial support of development, implementation and maintenance of SPHM programs may not be attained.
Collection and reporting of patient handling and mobility injuries must be easily implemented, concise and user-friendly to be sustainable. Above all, this proposed standard collection and reporting of more detailed data elements associated with patient handling and mobility injuries must also address the realities of the normal working environment and the various documentation requirements posed to the practitioner on a daily basis. In the era of big data, we must simplify the approach.
Future State: Keep it Simple and Transparent
Figure 2 provides a basic workflow for any healthcare system to investigate and adjudicate claims. The current U.S. workers’ compensation structure lacks uniformity across casualty claim service organizations related to patient handling and mobility injury identifiers. This inconsistency prohibits the ability to affect change through benchmarking or modeling at the local, regional and national levels. These critical data elements promote effective resource allocation, pre- and post-loss program development and implementation. Some of the key data elements not currently documented range from the most obvious, such as making an occupied bed, to other notable elements such as managing aggressive behavior. These causes provide the information to propel effective change and mitigate costs of these pervasive and many times debilitating injuries.
Other categories used to define specific types of movement and activities will create consistency across claims platforms as well as the much needed transparency for better injury cause identification and implementation of relevant, impactful solutions tied to the visible trends. This provides a mechanism to quickly and credibly identify a host of benefits:
- Trend injuries by patient handling task/activity (e.g. repositioning up in bed, limb holding, toileting, vehicle transfers)
- Identify predictive causes of injury
- Track frequency of specific injury types
- Effectively simplify big data into actionable elements
- Measure return on investment with SPHM programs
- Identify impact of patient handling and mobility equipment and programs
- Add additional dimension to the description of injuries
- Provide a method to benchmark outcomes
- Develop a sustainable best practice
Clearly the benefits demonstrate the need for moving forward with a simplified method. This approach will have a broad appeal as it closes a significant gap in the scope of the data being collected and allows SPHM professionals to compare data across peer groups in a consistent manner. Collecting more detailed information regarding the injury will also streamline RMIS coding constructs and allow providers to set up identical coding for all healthcare-related clients.
Figure 2: Current and Proposed Claim and Reporting Processes
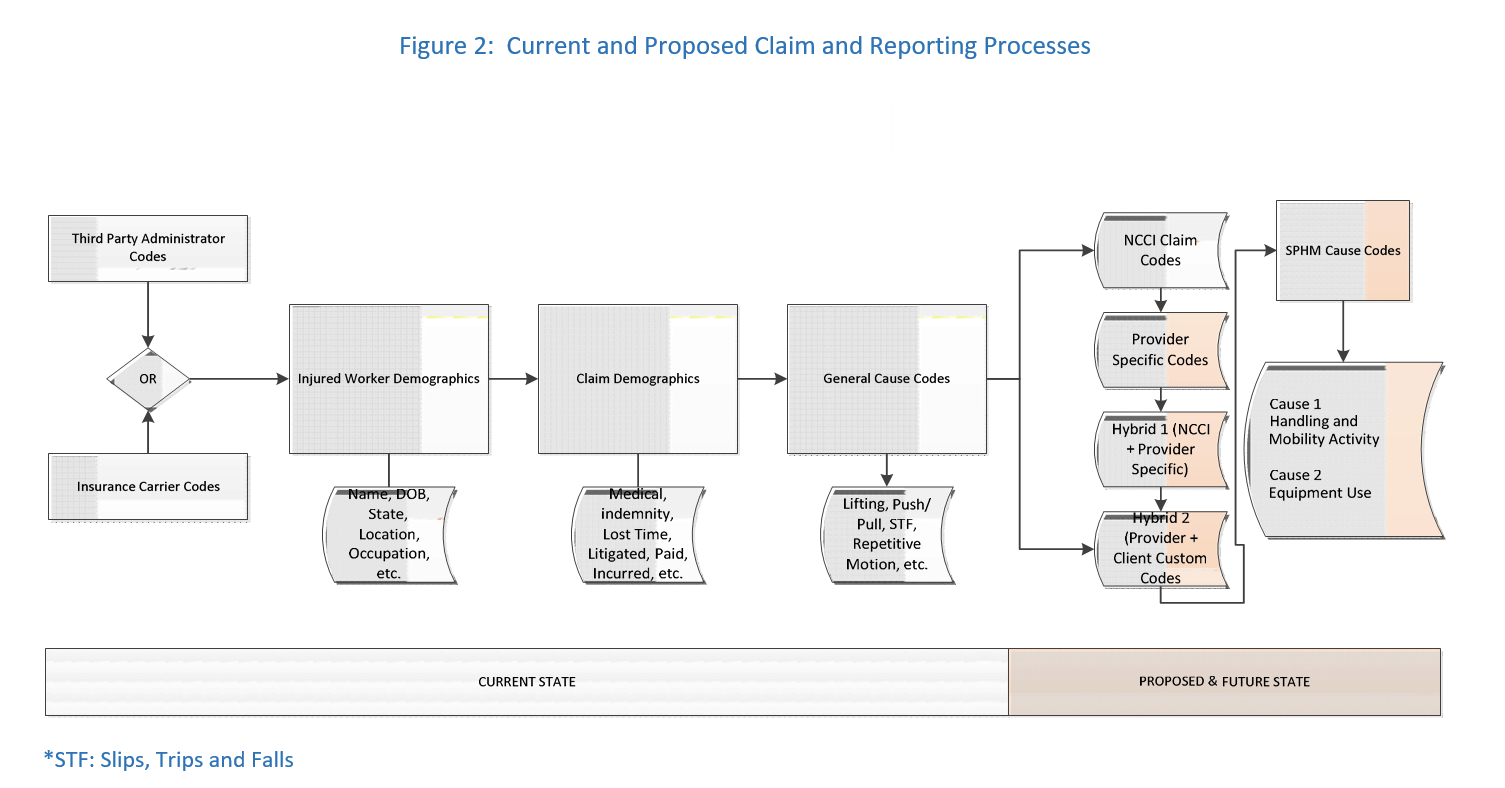
The detailed injury information proposed to be added to the intake process and RMIS systems will have a profound impact on the ability to extract actionable data elements. By instituting standard coding for the type of “Patient/Resident Handling and Mobility Activity” and “Patient/Resident Handling and Mobility Equipment Use” as shown in Table 2, risk managers or consultants to healthcare companies can retrieve actionable data from their claims administrators or internal systems.
Table 2 also shows the proposed national standard for additional elements, and it comprises a simple, yet easily implemented coding structure to add increased value to the claims intake and reporting process. By adding these critical categories, the benign loss run categories of “patient handling” or “strain—pushing/pulling” for example, bear more meaning and record vital information. (‘Patient’ is used in this paper to include all healthcare recipients; patients, residents, clients, etc.)
Table 2: Proposed Patient Handling and Mobility Injury Codes
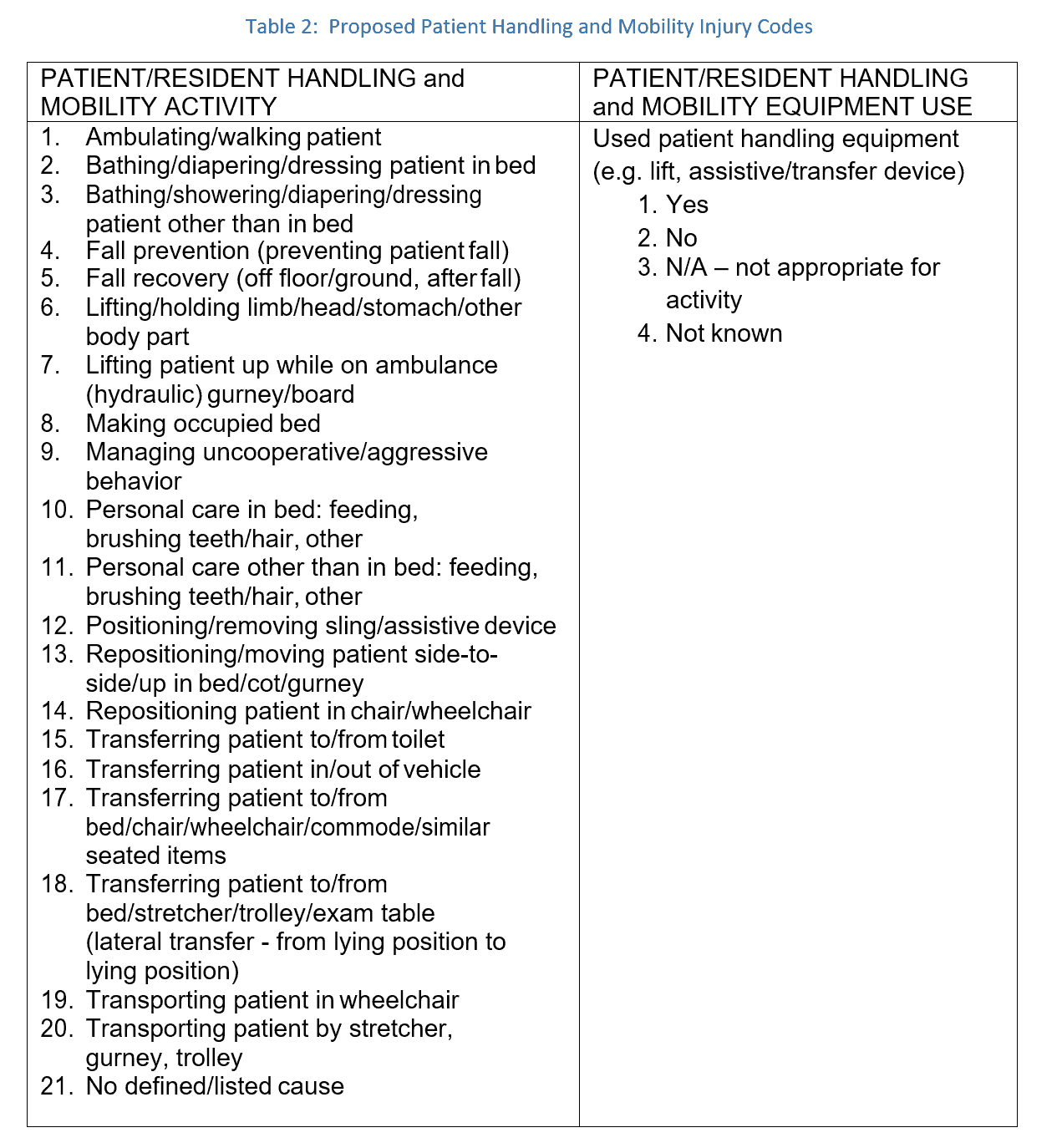
It is accepted that some patient handling injuries are difficult to classify and fall into the “no defined/listed cause (21)” category because they are cumulative in nature and may not have a specific cause. It is not uncommon to hear a caregiver say she has been lifting patients all day and now experiencing back pain. No specific task is identified as the cause nor can the caregiver suggest what caused the pain or injury other than, “lifting patients all day.” Such cumulative injuries are included in the “no defined/listed cause” sub-code. Additionally, RMIS includes cumulative trauma as a cause, so that code was not included in the proposed structure. Importantly, although cumulative trauma codes do not provide a clear understanding of what activity led to caregiver discomfort or pain, knowledge of trends in cumulative trauma provides actionable data in and of itself.Table 2 shows the codes defining patient handling, which will provide a clearer picture of the injury the caregiver experienced while performing a specific patient handling and mobility task. These definitions are supported by other incident reporting systems (e.g. NIOSH, Veterans Health Administration (VHA), etc.). Only a single code is required from each column. Ultimately, the data will provide information that may point to a single causative factor for that injury, such as the use or non-use of a SPHM assistive device.
Some workers’ compensation personnel may not be entirely familiar with the range of equipment used to support SPHM including ceiling and floor-based lifts, air-assisted lifting and lateral transfer devices, slippery sheets, friction reducing devices, roller boards, powered wheelchair/bed movers, powered toilet lift seats and more. Some beds, stretchers and gurneys are also included as SPHM equipment when they perform functions to help move and handle patients. However, walking aids such as walkers, canes, and crutches, as well as push wheelchairs and fixed or manually adjusted beds/trolleys/gurneys are NOT considered SPHM equipment. Slings (Table 2, Item 12) are used with patient lifting equipment to move and/or lift a patient or body part.
Stakeholder Value
Evidence-based information clearly demonstrates that certain categories of the data are linked to cost drivers. It is important to effectively utilize that information to more globally understand the overall results. Understanding the collection, reporting and data available to SPHM injury stakeholders and the impact that this information will have is imperative. The information in Table 3 will guide the improvement of the SPHM program functioning overall and reduce the negative effects of unnecessary patient handling and mobility injuries.
Table 3: List of Stakeholder Benefits and Corresponding Details
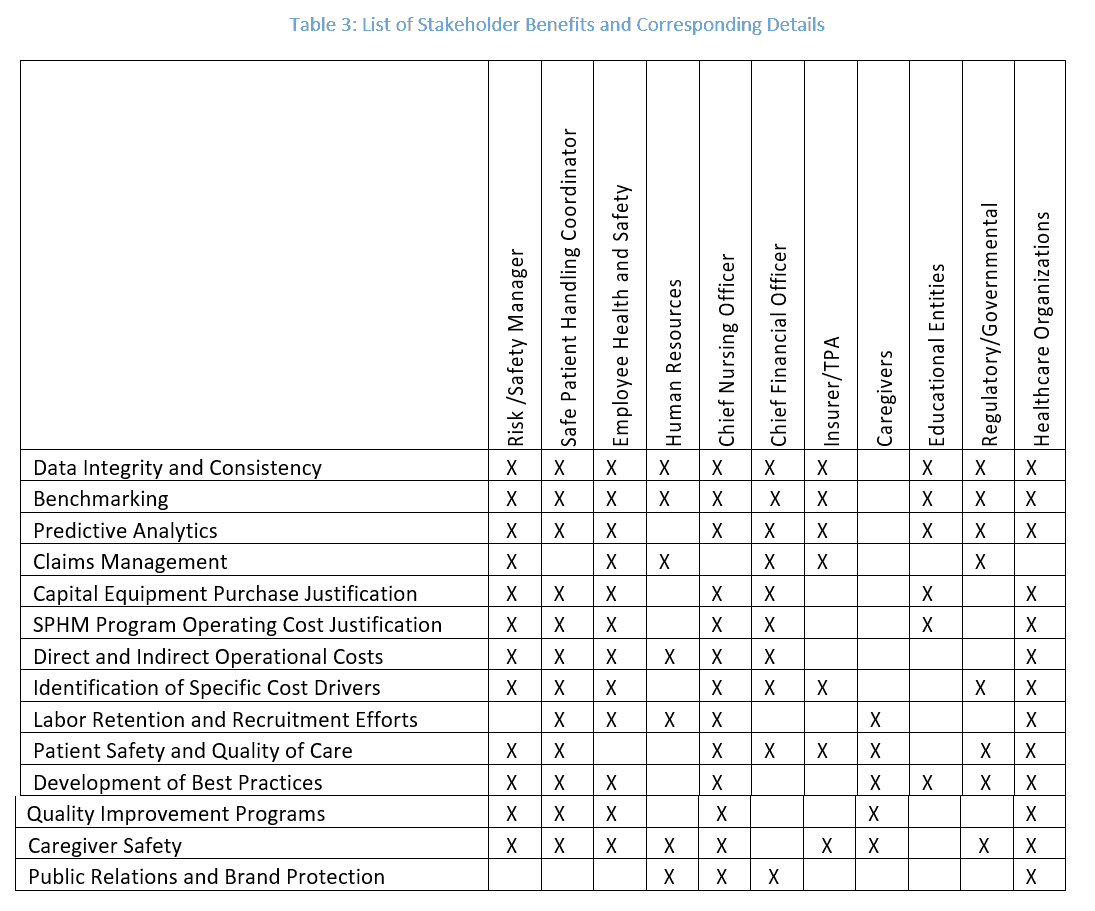
When Table 3 was developed, each of the named stakeholders’ perspectives was assessed through its own respective lens. For the reader to clearly understand how standardization of coding will impact each of the named stakeholders, a brief description and situational illustration is offered for each label in Impact of Coding Improvements.
Impact of Coding Improvements
Data Integrity and Consistency – Accurate, complete and concise capture and report of all requested data elements. Without standard data elements that are practical to obtain and easily recorded, the risk of incomplete and inaccurate information increases, reducing the possibility of any analysis or conclusions to be drawn organizationally or nationally.
Benchmarking – Comparing one’s SPHM program and performance metrics to industry bests or best practices. Comparative analysis provides a point of reference to internal and/or global results that may be either compared or assessed. Benchmarking provides a method through which each organization/facility may measure its SPHM program success against that of others; providing information to facilitate change.
Predictive Analytics – Extracting information from existing data sets to determine patterns and predict future outcomes and trends. Through the use of a set of standardized data elements, these trends may be used to draw sound conclusions and provide direction for future program decisions, such as determining SPHM program and equipment needs.
Claims Management – Advice or services related to claims for compensation, restitution for loss or damage due to injury or illness incurred in the practice and performance of patient handling and mobility activities. Standardized data elements provide claim managers valuable information to complete a thorough investigation and adjudication of each claim.
Capital Equipment Purchase Justification – Typically capital equipment is defined as items of considerable value that have durability and that are used to provide a service or increase revenue over the lifetime of the item. This may also be considered a tangible corporate asset. For the subject at hand, the justification of capital equipment purchases may be considered the more significant obstacle to development of a SPHM program. Data collected as a result of customized coding identifies cost drivers that in turn provide justification and validation for SPHM program capital expenditures.
SPHM Program Operating Cost Justification – Operating costs are expenses related to the operation of a business, or to the operation of a device, piece of equipment, or facility. They are the cost of resources used by an organization to maintain its existence. SPHM Program and equipment costs are considered operating costs. In healthcare, there is much competition for these funds. For this reason, there must be iron-clad justification/s for SPHM program and equipment costs. SPHM justification must include direct and indirect SPHM operational costs including equipment, staff training, staffing, and others. As well, benefits and cost savings for both patients and staff must be included. Staff cost savings relate to decreases in the rate of injuries, lost time, and modified duty injuries. Decreases in patient adverse events result in huge cost savings for an organization when there is an effective program.
Direct and Indirect Operational Costs – Direct costs of medical care (including rehab), indemnity (lost wages) and legal services are only several line item expenses to consider when assessing the fiscal impact of a musculoskeletal workers’ comp injury incurred due to SPHM activities. To be included with these obvious core costs are other expenses that must be accounted for when evaluating at the entire monetary effect of these injuries. Professionals also acknowledge injury indirect costs which include wages paid to injured workers for absences not covered by workers’ compensation insurance; administrative time to investigate the incident and perform other related supervisory duties; employee training and costs for replacing the injured workers; and lost productivity and accommodation of injured workers. While specific stakeholders are able to use data on certain line items to provide financial and other useful information, all stakeholders need to see the full picture of how SPHM injuries can affect the facility’s fiscal health and overall employee satisfaction.
Identification of Specific Cost Drivers – Specific activities or actions that have been identified to have costs associated to them. Customized coding will provide detailed activity descriptions to allow quantification of data and associated costs resulting from injuries.
Labor Retention and Recruitment Efforts – Data supports the fact that successfully competing for educated, trained and experienced healthcare workers in today’s market does not just depend upon wages, salaries, benefits, work shifts or available days off. Musculoskeletal injuries, cumulative or traumatic, have a significant effect on the professional and personal lives of the injured. Some injuries can disable and/or destroy a career. Competent caregivers also acknowledge that their safety and health closely relates to the welfare of their patients/residents. Having a SPHM program in place within a culture of safety demonstrates to recruits and affirms to current employees that the facility supports and protects them.
Patient Safety and Quality of Care – Currently, organizations must pay for negative patient outcomes related to hospital stays. Increasing evidence points to the importance of mobilization of all patients in the recovery process, which patient handling equipment facilitates. Falls, skin breakdown, UTIs, pneumonia, and other hospital-acquired injuries/illnesses are positively impacted when SPHM programs foster equipment use.
Utilization of Best Practices – There are tried and true processes for SPHM program development, implementation and maintenance. The ANA Safe Patient Handling and Mobility Interprofessional National Standards relay those national experts agree upon. The Veteran’s Health Association has the largest and most successful SPHM program in the United States, incorporating best practices found to be valuable in other organizations as well. When these best practices are supported, patient and staff injuries are impacted positively.
Quality Improvement Programs – This specific and defined process-based, data-driven approaches to improving the quality of a product or service are significant in all modes of healthcare provision. In the context of this paper, patient handling injuries drive many of the quality improvement programs’ focus. Customized coding will provide a consistent method from which data may be obtained and analyzed in the context of performance-based measurements.
Caregiver Safety – Occupational health and safety programs continue to identify risk factors and specific interventions to mitigate injuries due to patient handling. Rates of musculoskeletal injuries from overexertion in healthcare are among the highest when compared with other industries. A primary focus of this paper is to identify those data elements, which will provide sound and reproducible data to drive the continued development and improvement of SPHM programs.
Public Relations and Brand Protection – Communication systems provide immediate and up-to-date information to the consumer seeking products or services. These channels, whether newswires or social networking sites, provide the conduit for widespread public relations and positive branding. Public acknowledgment and reporting of a SPHM program developed, installed and maintained in the facility bespeaks the culture of safety that has been promoted and secured by administration. Knowledge that the facility cares not just for the patients/residents but also for the employees focuses on the humanity of the healthcare entity and instills consumer trust.
Engagement Blueprint
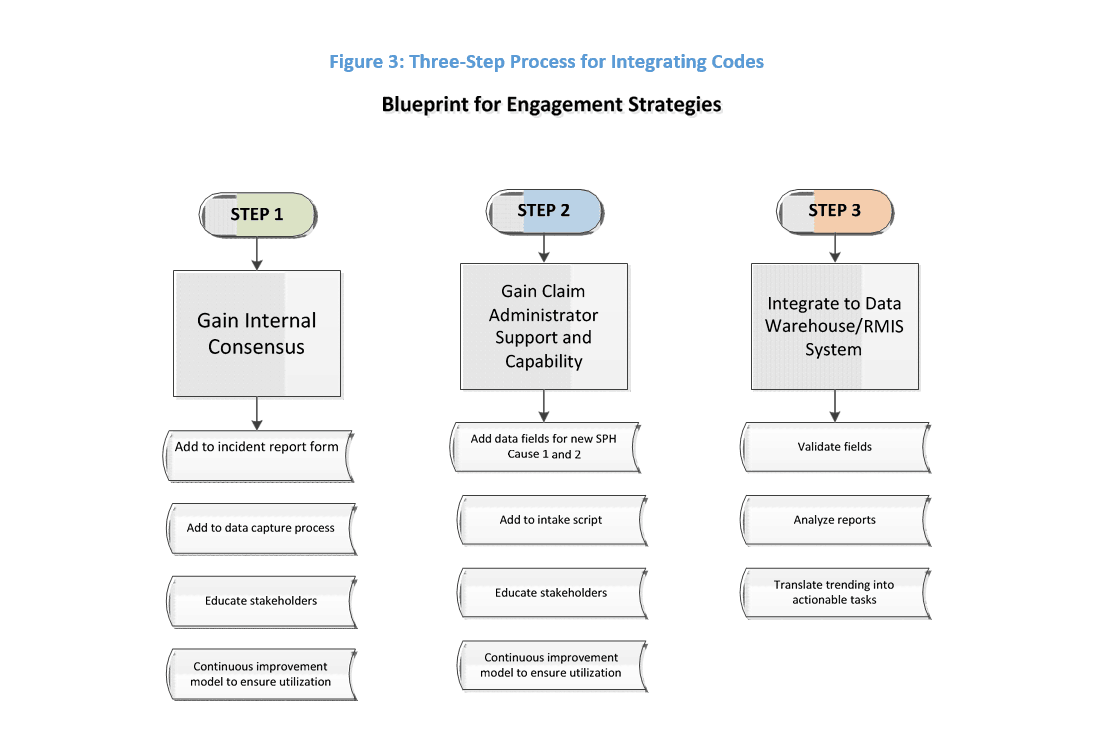
To gain consensus and buy-in for consistent coding, first think and act locally, then move to global applications. Figure 3 shows a simple process for adopting the proposed category in a gradual yet meaningful way. Step 1 involves adding proposed codes to the incident reports and other data capture processes to get consistent points adopted on the front end. As with any change, stakeholder education is critical. Steps 2 and 3 are at the administrator level, whereby stakeholders gain approval to institute the new coding in RMIS or other data capture systems. For example, adjustments to intake scripts would need to include the new coding, ensuring these questions are answered at the claim-reporting level. Because the new coding is simple in nature, there should be minimal impact to a data warehouse/RMIS system.
A Call to Action
Early adopters of more detailed coding practices have clearly demonstrated a positive impact on overall loss costs when compared to those that have yet to embrace this practice. These organizations are likely to garner peripheral and significant benefits such as staff retention, attraction of clinical talent in an environment with skilled nursing and medical professional shortages and productivity drains to name a few. However, administrators require tangible metrics to support the business case for development and maintenance of robust SPHM programs.
Ongoing state legislative activities are gaining momentum to encourage development, adoption and standardization of programs. This movement will likely continue. Federal adoption and support of SPHM standards and practices have yet to be enacted. However, without a standard from which to measure outcomes, comparison and trending, enumerable losses will continue. Moving forward, stakeholders will need to take a pragmatic and incremental approach to engage all participants in the process. As engagement increases and results are measured, further expansion of codes may be introduced as practically appropriate.
Conclusion
Fundamentally, caregiving is a humanitarian effort based on respect and concern for others. As science and the ability to treat and cure has progressed through the years, longer lives lived with chronic, debilitating and frail conditions and the needs for more challenging rehabilitation efforts have resulted.
The caregiving workforce and the patients/residents are all aging. And more than ever, the condition of the financial bottom line is tenuous and difficult to control.
It can easily be acknowledged that the implementation of a successful SPHM program, led by an expert in the field and supported by others who are educated and experienced in the scope and practices of the program, makes a significant difference in the health and welfare of the caregivers, the cared-for and the service-providing entity.
Be reminded of Table 3, illustrating the value of this proposition, and all the ways that patient handling and mobility injuries can negatively affect lives, jobs and the bottom line. The proposal for standardized coding herein is simple and easy to implement so that healthcare organizations can maintain the practice and contribute meaningfully to decreasing staff injuries, improving patient/resident care and prolonging solid careers.
With inclusion of the proposed categories, improved data and its analysis will become consistent and available to all; providing the information necessary to improve safety programs. Assistive patient handling and mobility equipment is available and will continue to improve when the exact needs for the implicated tasks are consistently coded and brought to light.
References
- American Nurses Association (ANA). (2013). SPHM Interprofessional National Standards Across the Continuum. Publisher: Nursebooks.org. Silver Springs,
- National Institute for Occupational Safety and Health coding system [Occupational Health Safety Network (OHSN) (2015) http://www.cdc.gov/niosh/topics/ohsn/injury.html
- Bureau of Labor Statistics 2014 BLS Newsletter 2014. http://www.bls.gov/news.release/archives/osh2_12162014.pdf
- S. Department of Labor, Occupational Safety and Health Administration. (2013). Hospital eTool: Healthcare Wide Hazards – Ergonomics. Available at: https://www.osha.gov/SLTC/etools/hospital/hazards/ergo/ergo.html. Accessibility verified 1/29/2016.
- Institute of Medicine (IOM) (2011). Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: The National Academies
- National Institute for Occupational Safety and Health (NIOSH). NIOSH Standard Occupational Data Architecture (SODA 2.0) Draft document dated June 24,
- Khatutsky, G., Wiener, J. M., Anderson, W. L., & Porell, F.W. (2012). Work-related injuries among certified nursing assistants working in US nursing homes. RTI Press publication No. RR-0017-1204. Research Triangle Park, NC: RTI Press. Retrieved from rti.org/rtipress.
Disclosure Statement
The Association of Safe Patient Handling Professionals (ASPHP) does not endorse one particular company or organization. Reference within this paper to any specific commercial or non-commercial product, process, or service by trade name, trademark, manufacturer or otherwise does not constitute or imply an endorsement, recommendation, or favoring by the ASPHP.
The views and opinions of the authors of content provided in this paper do not necessarily state or reflect the opinion of the ASPHP and cannot be used for advertising or product endorsement purposes.
Acknowledgments
All of the authors of this white paper are members in good standing with ASPHP and serve as Board members. Wendy Weaver is the past Executive Director of the organization.
Mike Fray PhD, BSc(Hons), BHSc, MCSP, FHEA Senior Lecturer
HEPSU, Design School, Loughborough University UK
Vicki Missar, MS, CPE, SSBB, CSPHP, CHSP
Associate Director, Global Risk Consulting Aon
Candy Raphan, RN, BSN, ARNP-C, MAOM Regional Vice President
Client Services Medical Management Broadspire®
Mary Matz, MSPH, CPE, CSPHP
Patient Care Ergonomics Consultant President, Patient Care Ergonomic Solutions
Wendy Weaver, MEd
Gateway Coaching & Consulting, LLC