
America claims less than 5% of the world’s population, yet it consumes roughly 80% of the world’s opioid supply. Knowing the potential for misuse of these medications, and facing an increase in opioid-related deaths in this country, we wanted a deeper understanding of how patients in the U.S. are using these medications so we can identify additional ways to protect them from the risks associated with their use.
In A Nation in Pain, our research revealed a drop in short-term use of opioids, and stabilization in the number of patients using these medications longer term, which is in contrast to the increases seen in the past. Both trends indicate that doctors are being more cautious about prescribing these pain medications.
However, the research uncovered some concerning increases in the amount of prescription opioid medications Americans use, and the frequency in which these medications are used in dangerously high doses and in risky combinations with other medications.
Prescription Opiate Trends Increase Potential for Abuse
Nearly 60% of patients taking opioid pain treatments for long-term conditions were prescribed potentially dangerous mixtures of medications during the same time period. Two-thirds of patients using these medication mixtures were prescribed the drugs by two or more physicians, and nearly 40% filled their prescriptions at more than one pharmacy.
Among those taking dangerous drug mixtures last year:
- 27% were taking multiple opiate pain treatments simultaneously.
- Nearly 1 in 3 patients were on an opiate and benzodiazepine (an anti-anxiety medication), a combination that is the most common cause of multiple drug overdose deaths.
- Approximately 28% took both a prescription opioid and a muscle relaxant, and 8% were combining an opioid, muscle relaxant and a benzodiazepine. Opioids, muscle relaxants and benzodiazepines all have sedating effects and can slow down the respiratory system. Taking these medications together could increase these reactions exponentially.
- Women accounted for nearly two-thirds of those taking these potentially hazardous mixes of medications.
Although there could be instances in which prescribing an opioid in combination with these other medications is appropriate, evidence of this concurrent use at such a large scale – and involving multiple prescribers and pharmacies – indicates there could be a breakdown in communication among a patient’s care team or potential abuse.
Also concerning was the discovery that nearly half of patients who took opiate painkillers for more than 30 days in the first year continued to use them for three years or longer. In addition, almost half of chronic opioid users took only short-acting medications – rather than longer-acting formulations – thus increasing their risk for addiction.
Prescription Opiate Use Most Prevalent in Southeastern Small Cities
According to the report, the number of Americans using prescription opiates declined 9.2% in the past five years, yet both the number of opioid prescriptions filled and the number of days of medication per prescription rose more than 8% between 2009 and 2013.
PREVALENCE OF SHORT-TERM AND LONGER-TERM OPIATE PAIN MEDICATION UTILIZATION

Of the 25 cities with the highest prevalence of longer-term opioid use, 24 have populations fewer than 100,000. On average, 3.9% of Americans were using prescription opioids on a longer-term basis in 2013; in small cities, that average is significantly higher at 5.1%
.
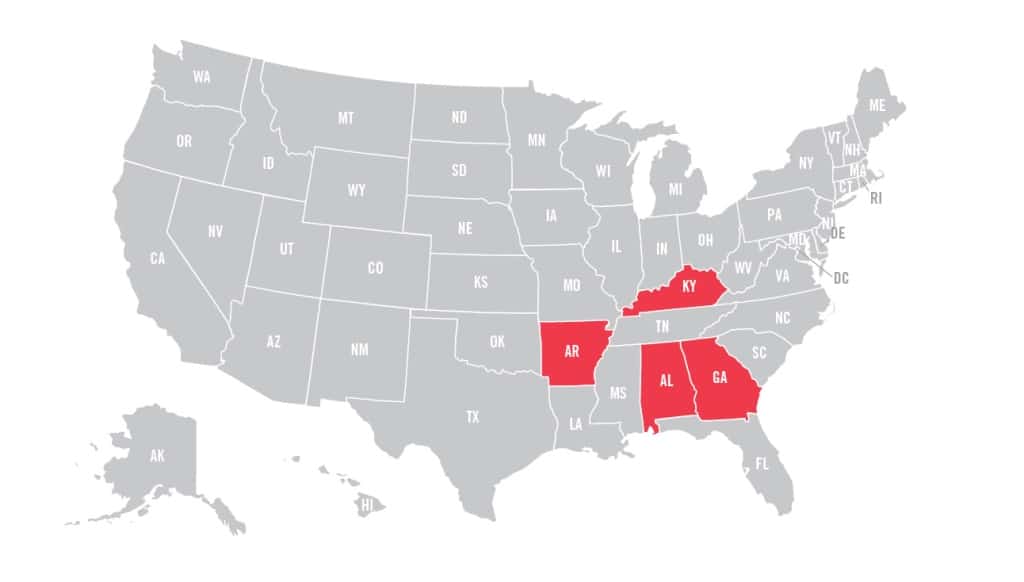
Among small U.S. cities with fewer than 28,000 residents, the top five had between 12.3% and 18% of their population using prescription opioids and were located predominately in Alabama, Arkansas, Georgia and Kentucky.
STATES WITH THE HIGHEST AVERAGE PREVALENCE OF OPIOID USE
Express Scripts Protecting Patient Safety and Preventing Abuse
Prescription opioids can provide patients with clinically safe and effective pain management. However, the potential for misuse and addiction requires vigilance and exemplary coordination of care.
When patients use home delivery to fill their prescriptions through the Express Scripts Pharmacy, they are cared for by specialist pharmacists with advanced training in pain treatments who can identify cases of suboptimal pain management and help patients use opioids safely and effectively. A subanalysis of the research shows that when compared to those who filled their prescriptions at a retail pharmacy, 23% fewer patients who filled their medication through the Express Scripts Pharmacy were using a potentially dangerous combination of medications, and 15% fewer patients were prescribed medications by multiple prescribers.
Express Scripts’ Fraud, Waste and Abuse program identifies potential cases of drug abuse, conducts extensive investigations and recommends interventions where necessary. The rate of concurrent use of potentially dangerous medications was 7.6% less in patients whose benefit plan was enrolled in the Express Scripts Fraud, Waste and Abuse program in 2013 compared to patients whose benefit plan was not enrolled in the program.
Research Methodology
For the report, Express Scripts examined 36 million de-identified pharmacy claims of 6.8 million commercially insured Americans of all ages who filled at least one prescription for an opioid to treat acute or longer-term (nonacute) pain from 2009 through 2013. Prevalence, use and costs were evaluated during the five-year study period, including assessments of trends according to age, gender and geography. The research also looked at users prescribed opioids in combination with other medications.



















