Putting new lifesaving medicines within reach requires novel collaboration. In approving …
Prescription Drug Use & Abuse
7 Ways to Reduce Your Workers’ Comp Prescription Drug Spend
Focusing on generics instead of brand name drugs, and in-network pharmacies instead of …
7 Ways to Reduce Your Workers’ Comp Prescription Drug SpendRead More
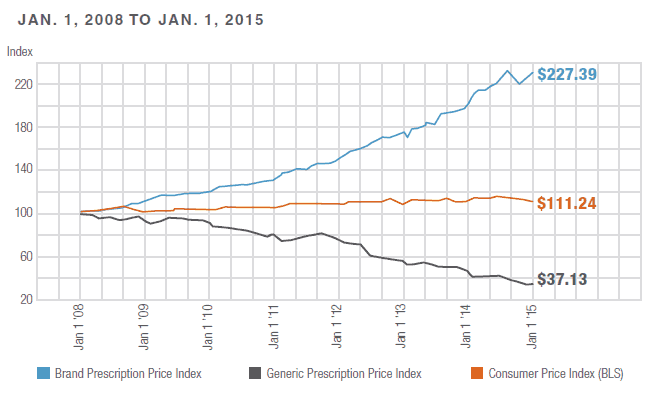
Increase Generic Fill Rate to Eliminate Wasteful Pharmacy Spend
Here’s a sobering statistic: “the average price for the most commonly used brand-name drugs has …
Increase Generic Fill Rate to Eliminate Wasteful Pharmacy SpendRead More
Why “Abuse Deterrent” Is A Misnomer
Instead of mandating first-line coverage for ADF opioids, we must remain committed to reducing …
Leverage Pharmacy Controls to Reduce Opioid Spending 13.4%
The workers’ compensation industry has been a leader in addressing the national opioid epidemic. …
Leverage Pharmacy Controls to Reduce Opioid Spending 13.4%Read More
Express Scripts & myMatrixx Combine to Offer Best In Class Pharmacy Services
ST. LOUIS, May 17, 2017 /PRNewswire/ -- Express Scripts (NASDAQ: ESRX) today announced it is taking …
Express Scripts & myMatrixx Combine to Offer Best In Class Pharmacy ServicesRead More
Kicking the Opioid Problem: 5 Steps to Keep the Train Moving
There’s been some good news about opioid challenges in the workers’ compensation system lately. The …
Kicking the Opioid Problem: 5 Steps to Keep the Train MovingRead More
Workers’ Compensation Prescription Drug Spending Decreased 7.6% in 2016
St. LOUIS, Apr. 4, 2017 – Express Scripts (NASDAQ: ESRX) lowered prescription drug spending for …
Workers’ Compensation Prescription Drug Spending Decreased 7.6% in 2016Read More
WCRI Recap: Single Biggest Factor To Turn-Around Opioid Crisis
WCRI Recap - 3 Part Series WCRI Recap - Impact of Donald Trump and 2016 Election WCRI …
WCRI Recap: Single Biggest Factor To Turn-Around Opioid CrisisRead More
4 Questions On Urine Drug Testing To Deliver Better Work Comp Outcomes
Urine drug testing (UDT) is one of the more controversial and misunderstood tools in the workers’ …
4 Questions On Urine Drug Testing To Deliver Better Work Comp OutcomesRead More
Opioid Addiction: The Painful Reality
For years, Express Scripts has been committed to managing concerns about long term opioid use, …
America’s Pain Points
Express Scripts’ newest report, A Nation in Pain, provides a comprehensive examination of the …
Chronic Pain: A Double Dose of Trouble
Dealing with “chronic pain” is an issue the workers’ compensation claims management team deals with …
Chronic Pain Management: 3 Tips to Help Injured Workers Avoid Opioid Addiction
Managing chronic pain with today’s medical advancements can mean a very high risk of addiction to …
Chronic Pain Management: 3 Tips to Help Injured Workers Avoid Opioid AddictionRead More
Stopping the Opioid Drug Epidemic In Workers’ Compensation
The opioid-based drug epidemic is causing havoc across the United States. It is also leading to …
Stopping the Opioid Drug Epidemic In Workers’ CompensationRead More
Stopping Opioid Abuse Through Effective Communication
The main driver in the cost of workers’ compensation claims remains the medical aspects of the …
Stopping Opioid Abuse Through Effective CommunicationRead More
Reality Check on Generic Prescription Drug Costs
The use of generic drugs in workers’ compensation is an effective and efficient method for …
Control Opioid Abuse With Morphine Equivalent Dose Program
The use and abuse of narcotics in workers’ compensation has exploded over the past decade, creating …
Control Opioid Abuse With Morphine Equivalent Dose ProgramRead More
Use of Drug Formularies to Reduce Workers’ Compensation Costs
The California workers’ compensation system may soon see some relief from the rising costs of …
Use of Drug Formularies to Reduce Workers’ Compensation CostsRead More
The Face and Cost of Opioid Addiction
The face of addiction is often perceived as not a pretty sight. The "normal" people of …