I always laugh when I hear my friend talk about the fact that “Big brother is watching us.” …
Surveillance Cameras Can Make Difference In Work Comp ClaimsRead More
I always laugh when I hear my friend talk about the fact that “Big brother is watching us.” …
Surveillance Cameras Can Make Difference In Work Comp ClaimsRead More
Adjuster Will See Thousands of Claims Throughout the course of an adjuster’s career they will …
Is Your Adjuster Playing Favorites With Your ClaimsRead More
Best Practices Approach to Post-Loss Costs Containment. A solid workers’ compensation cost control …
Identify Real Cost Drivers in Post Loss Workers CompensationRead More
Deer Season Can Equal Spike in Work Comp Claims Fall has arrived. Time is say goodbye to days at …
It is Deer Hunting Season, Be Aware of a Spike in Work Comp ClaimsRead More
According to a new report from New Hampshire’s Department of Health and Human Services, merely half …
Many Injured on Job in New Hampshire Did Not Receive Workers Comp CoverageRead More
We often hear about “best practices” for workers compensation claims-handling …
Three Areas Where Best Practices for the Employer Can Make a DifferenceRead More
Some thoughts on whether being "average" is good enough... What does it cost to buy a …
To maximize your company’s potential for workers’ comp cost containment we recommend …
Eight Focus Areas for Best Practice Cost Containment of Workers CompensationRead More
Small changes in your workers’ compensation program lead up to large cost savings. Your company’s …
Assessment is Your Number One Tool for Cost ControlRead More
From time to time an external claims auditor comes across a workers' compensation claim approaching …
15 BEST PRACTICES Picture Perfect Handling of a Workers Comp ClaimRead More
While there are a variety of programs to reduce workers' compensation costs, there are …
Does YOUR Company Use These 5 Basic Practices to Lower Workers Comp CostsRead More

Communications, is key to good inter-personal relationships. Communicating is even more critical …
Supervisors are the front-line reporters of work-related injuries and accidents and bear the …
What are Supervisors Best Practices When Handling Workers Comp Related InjuriesRead More
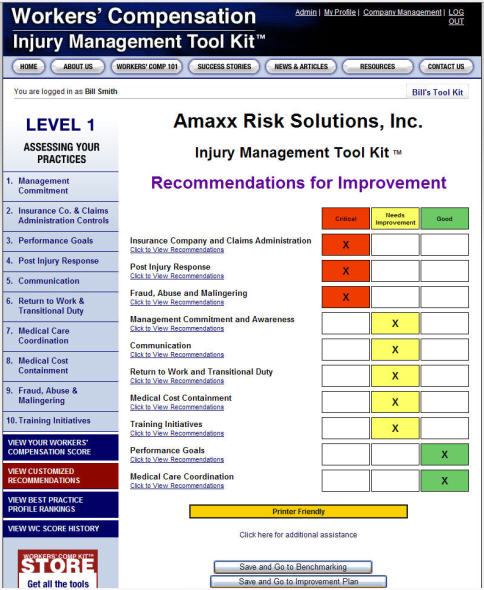
When improving your workers' compensation programs, it's important to prioritize the …
Prioritize Best Practices in Workers Compensation ProgramsRead More
As a productive member of your workforce, employees must participate in your Workers' …
Nine Employee Responsibilities in Best Practice Cost Containment ProgramRead More
Our National Workers' Compensation Management Scores™ are numeric scores ranked for 1-100. Yes, you …
National Workers Compensation Management Scores™ are Quantifable — Best Practices MeasuredRead More
